Thoracoscopic Esophageal Atresia Repair First Ever Pakistanian Study, Early Learning Curve-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Introduction
Esophageal atresia with or without fistula is rare congenital anomaly occurring In 1/3000-5000 of neonatal population [1]
which is traditionally repaired by posteriolateral thoracotomy&
still a standard approach, but this approach is associated with
musculoskeletal morbidity and later in life scoliosis, chest wall
deformity & nerve damage [2-4].
With the advancement in minimal invasive paediatric procedures &
high definition technology and looking into consideration of these
morbidities it become possible to perform technically demanding &
complex procedures thoracoscopicaly. In relation to this first time in
1999 isolated esophageal atresia done in male infant of 2 month which
was repaired thoracoscopicaly [5]
For last 10 years after first repair refinement's in
technique & feasibility in thoracoscopic repair of esophageal
atresia led to adoption of this technique in many institutions world
wide [1]
The objective of study is to do esophageal atresia
thoracoscopicaly going through few basic steps of learning curve to make
it possible for achievement of final thoracoscopic repair
Material and Methods
This is retrospective study conducted from June 2015
to May 2016 at Peoples University of medical & health sciences
Nawabshah Sind, Pakistan & 11 patients included for thoracoscopic
esophageal atresia repair Detailed pre-operative assessment done in all
patients, fullterm with type C esophageal atresia weighing greater than
1.5 kg was selected. Neonates with major cardiac anomalies on
echocardiography & having GI anomalies were excluded. Preoperative
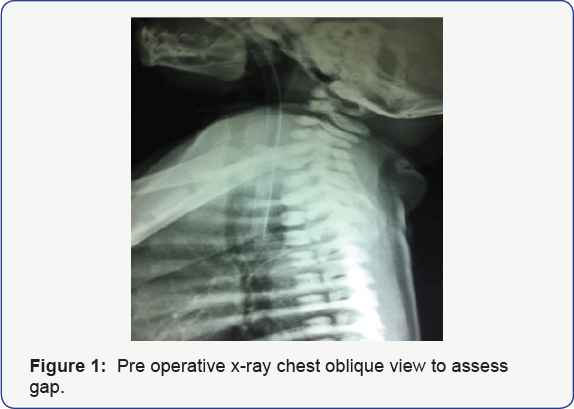
assessment of gap between two atretic ends were roughly assessed by
plain x-ray of cervical & thoracic spine in lateral view with large
bore tube in situ in esophagus.The distance between tube & expected
carina level at T4 measured and if it is more than two vertebrae
expected to be larger gap between two ends (Figure 1)
Data collected included newborn age & weight at the time of
surgery, operative time, mechanical ventilation required, days of
hospitalization, time to start first feed & post-op complications.
Technique
Baby placed in modified prone position with right
side elevated at 45 degree with tracheal intubation in all cases &
no attempt was done for single lung ventilation. In first four cases
single small incision of 2-3 cm like we do in VATS given below the tip
of scapula at 5th intercostal space. 5mm scope put from top
of incision & two working 3mm instruments places directly from mid
of incision, lung retraction done with 3mm fan retractor from bottom of
incision .The aim of this technique was to see videoscopic view of
internal anatomy and to assess difficulties while doing few of steps
video-asisted like azygos vein ligation & fistula dealing. Rest of
procedure completed by open method. In next 7 cases three port technique
was used consisted of camera port of 5mm just below tip of scapula,
right port of 5mm In mid axillary line two space above camera port and
the last 3mm port placed two space below in 6th or 7th intercostal space behind posterior axillary line (Figure 2).


Lung collapse was done with Co2 insufflations with
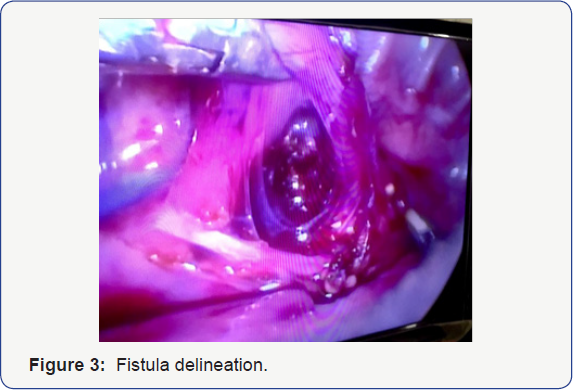
flow of 1lit/min & pressure kept between 5-8 mmhg. The first step in
all cases was to deal azygos, which was accomplished by hook electrode
easily after opening the pleural membrane. Next step was to ligate with
fistula (Figure 3) which was done with 5mm of Grena plastic clips passed through right upper port (Figure 4)Next
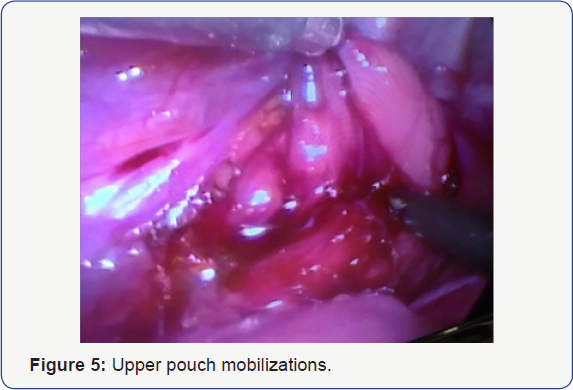
was to identity the upper pouch, which was mobilized by hook in right
hand and grasper in left hand to pull pouch inferiorly to achieve
adequate length (Figure 5)
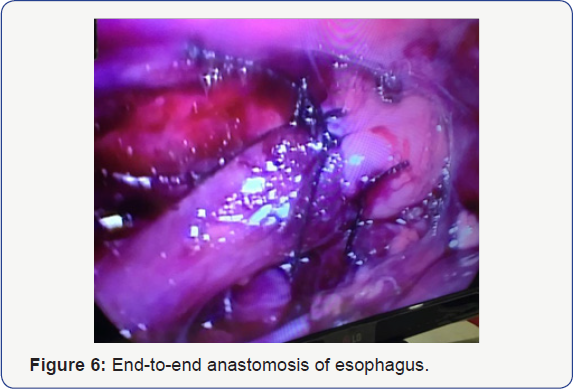
Once the good length is achieved posterior layer of two ends was done
intracorporeal by 5/0 non-absorable in 2 cases and vicryl in rest of
cases. After completing posterior layer trans anastomotic tube placed
& anterior layer of esophagus repaired (Figure 6) Chest drain placed in all cases.
Results
Initial 4 cases out of llcases underwent video
assisted like Uniportal VATS, which were later on converted to complete
the procedure &7 cases, were successfully done thoracoscopicaly.
Mean age at the time of surgery was 3 days because most of patients
coming late in our hospital & mostly they are diagnosed postnatally.
Weight of patients at the time of surgery ranges between 1.5-3.5kg in
the initial case as including the video assisted cases the operative
time was bit longer between 120 to 150 minutes, which later on improved
in last two cases was under 120 minutes. Mechanical ventilation required
in 4 cases &rest of patients were fine post operatively and only
required oxygen support for few days.
Contrast swallow done in all case on day 5 but in 2
cases early contrast was done suspecting leak out of which one case had a
confirmed leak, which was healed conservatively. First feed was started
on day 3 in 4 cases through nasogastric tube which were clinically
fine, in 5 cases feed started on day 5 after contrast swallow &
remaining two case feed started lately after 6 days as these were on
mechanical ventilation.
Postoperative complications encountered in 3 cases
out of which one had leak, one had stricture & last one had reflux.
Leak was managed conservatively, stricture improved on dilatation &
gastro esophageal reflux managed on medical therapy. Days of
hospitalization were variable ranging from 8 days to 16 days. There was
one mortality in our series that patient presented late after 7 days
& died because of sepsis.
Discussion
According to IPEG & EUPSA survey thoracoscopic
esophageal repair is a world wide accepted procedure in more than 65
developed centers that are attempting but many aspects of EA management
are lacking consensus they recommend establishment of an EA registry at
the end of survey [6,7] .
In few Asian countries & Middle East
thoracoscopic repair of esophageal atresia has been started but they are
at initial learning stage & they have found same results as develop
centers [8-10].
In Pakistan it is first ever study done which is going to be reported
in order to follow the develop centers doing advance paediatric minimal
invasive surgery. Details regarding advantage of thoracoscopic repair
have been extensively studied like superior visualization, Cosmesis,
identification of fistula & avoidance of musculoskeletal morbidities
[1,11].
In our study in the initial four cases we have adopted new technique
like Uniportal VATS to learn the videoscopic anatomy & to do
procedure keeping the safety of patient in mind. Regarding age, weight
& associated anomalies our selection criteria was safe as we have
excluded cases with low birth weight, prematurity & major cardiac
association are absolute contraindication to thoracoscopic approach as
Rothenberg et al also described in his studies [12].
Azygos vein ligation or sparing is an option, which
in our study in all case dealt with coagulating hook, but in few studies
azygos sparing technique have been done claiming lesser edema at
esophageal anastomotic site & prevention of recurrent fistula
formation [8,9,13].
Fistula ligation can be done in different ways like suture ligation,
titanium clips but we have done with Grena 5mm plastic clips which is
having secure locking mechanism in front but there is no statistical
significant difference in all techniques [1, 11,14].
The most difficult part of surgery is esophageal
anastomosis intracorporeally which is technically demanding, the
technique is same like open but the first stich is difficult one to
apply because of apart ends, we have the same feelings especially in
long gap where we have applied stays before applying first
intracorporeal stich [8,11].
The operative time is variable in our study which was more in initial
cases because of technical difficulty & small working space, the
same duration of operative time was seen in other studies with their
initial learning curve experiences.
Although the number of patients in our series is
small we cannot conclude issues related to post operative complication
like leak & anastomotic narrowing in our cases was only 10% each but
different comparative studies have found these complication are lesser
in thoracoscopy group versus open group [15,16].
Recently study by borruto et al with Meta analysis
shows no difference in open & thoracoscopic group but the only
advantage is to prevent major thoracotomy [17].
Conclusion
Thoracoscopic repair of esophageal atresia with TEF
is feasible, but is technically challenging& demanding.Our current
experience is on quite limited number of patients and there is
considerable learning curve required till the perfection of procedure.
There is need to make refinements in the steps of the complex paediatric
laparoscopic procedures to make it easy for surgeons wanting to adopt
this procedure. Take home message is that a multi center program should
be started in our part of world that should be guided by experienced
surgeons from developed centers& secondly advance suturing skills
should be learned before starting this procedure.Avoidance of
thoracotomy is a major advantage and is proven benefit in the recovery
of patient.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment