Outcome of 'CDC Kerala' Early Stimulation Model on Neurodevelopment of Late Preterm Infants-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
There is increasing evidence that late preterm babies
(Gestational Age 34-0/7wks to 36-0/6 wks) are at increased risk of
short term developmental morbidities as compared to term counterparts.
Cochrane review had shown that early intervention programs for late
preterm infants have a positive influence on motor and cognitive
development on short-medium term. Early intervention programs like
NIDCAP (Newborn Individualized Developmental Care & Assessment
Program), IHDA (Infant Health & Development Program) are best
evaluated. Parent based studies have shown positive influence on
neurodevelopment outcome. Present study assesses the outcome of parent
based early stimulation model on neurodevelopment of late preterm
infants by corrected age of 12months.
Keywords:
Late preterm babies; Neurodevelopment outcome; Early stimulation; Parent
based intervention; Developmental screening tools; Developmental
assessment scale for Indian infants
Abbreviations: CDC:
Child Development Centre; LP: late Preterm; DASII: Developmental
Assessment Scale for Indian Infants; DQ: Deviation Quotient; MeDQ:
Mental Deviation Quotient, MoDQ: Motor Deviation Quotient, BSID: Bayley
Scales of Infant Development; TDSC: Trivandrum Developmental Screening
Chart; DDST II: Denver Developmental Screening Test; A T angles:
Amiel-Tison angles
Introduction
The near term terminology has been replaced by late
preterm for babies born between34-0/7 to 36-6/7Weeks’ of gestational
age. This emphasizes that last 6 weeks of gestation represent critical
period of growth and development. Studies have shown that these babies
are at three times higher risk for morbidity and mortality than their
term counterparts [1,2].
Indian study done by Wagh & Jain reported higher neonatal
morbidities in LP babies like need for resuscitation, hypoglycemia,
feeding problems, sepsis and hyper bilirubinemia than term controls.
They shared concerns of growth and development at 3 months of corrected
age in these babies [3].
An inverse relationship between gestational age and risk of
developmental delay at 18 months of corrected age was found by Luisa et
al. [4].
With better understanding of importance of early
enrolment of these babies in early stimulation programmes, their
Neurodevelopment outcome has improved [5,6]. Systematic review done by Orton et al. gives account of various early intervention models for these babies [7]. CDC model of early stimulation is parent based, home cantered model which has shown its effectiveness in RCT [8]. Present study assesses effectiveness of this model on Neuro developmental outcome of LP infants.
Materials and Methods
Retrospective, cross sectional analysis of enrolled
cases between March & April 2014 which were followed up to 12months
of corrected age at CDC, Kerala.
A. Inclusion criteria: LP Infants (Gestational age 34-0/7 to 36- 6/7 weeks) attending CDC Newborn Follow up clinic.
B. Exclusion Criteria: Major congenital anomalies, visual and hearing impairments.
C. Sample Size: 53 late preterm babies.
D. Intervention & monitoring:
i. CDC model of early stimulation (ES) monthly till 12months of Corrected Age
ii. CDC model ES is indigenous, mother oriented
program,designed for babies 0-12months, executed by multidisciplinary
team. Its effectiveness is proven in RCT across all birth weight groups [8].
iii. Developmental Screening Tools - TDSC, DDST II, AT angles, CDC grading of major motor milestones.
iv. Simultaneous assessment of vision, hearing, lactation and feeding was done.
v. Home program: Hands on training on ES techniques
encompassing all developmental domains to mother/ care giver and
encouraged to do the same many times at home.
vi. Outcome Measure: Evaluation by DASII at 3-5 months (1st DASII) & 12 months (2nd
DASII) of corrected age- Mental age, Motor age & deviation
quotients derived. MeDQ, MoDQ value 80 and above were taken as normal as
and less than 80 as abnormal.
vii. Developmental Assessment Scale for Indian
Infants (DASII) is an Indian standardized adaptation of BSID to assess
motor, cognitive development of children up to 30 months of age.
Statistically analyzed with variables - weight,
gestational age, National Neonatology Forum (NNF- India) risk factors,
parent education and socioeconomic class (Table 1).
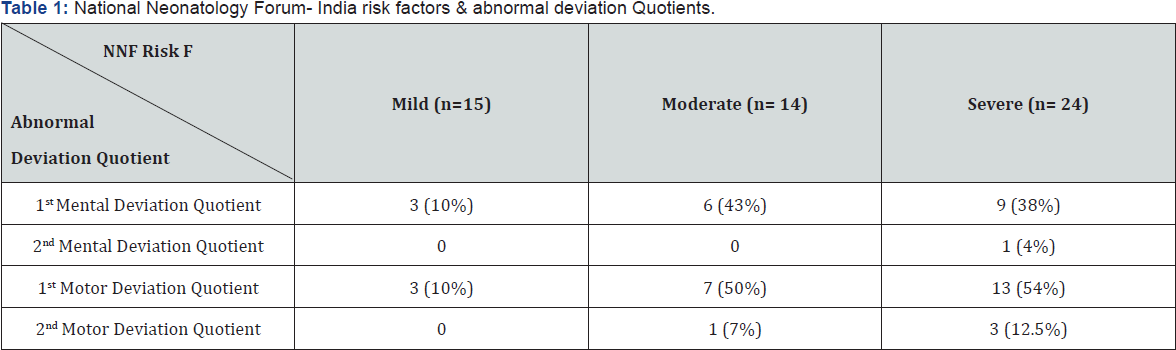
Babies with mild and moderate National Neonatology Forum- India risk factors had less abnormal Deviation Quotient.
Results
A. Total 53 babies satisfied inclusion exclusion
criteria. 53% (28) were males and 47% (25) were females. 40% (21) babies
were normal at 3, 12 months. With respect to socioeconomic class 43%
subjects were BPL (Below Poverty Line), 57% were APL (Above Poverty
Line). No parent was illiterate.
B. Mother Education- 10th std- 2, 12th std- 25, Graduation- 25, Post graduation- 1
C. Father Education- 10th std- 1, 12th std- 21, Graduation- 27, Post graduation- 4
D. Birth weight & Deviation quotients of DASII- (Table 2)
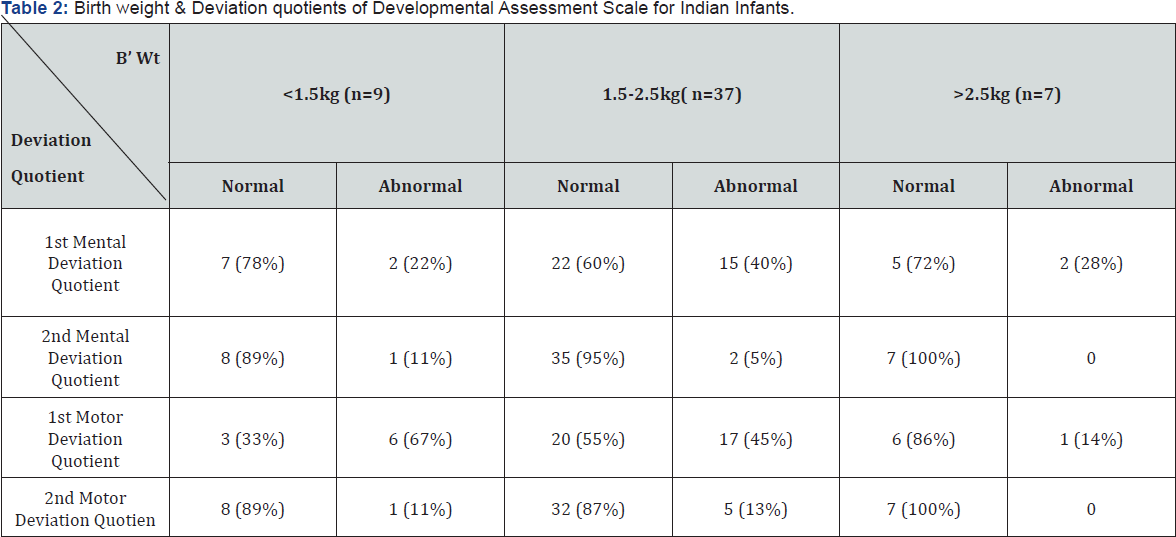
As the birth weight increases, percentage of abnormal Deviation Quotient decreases
E. As the birth weight increases, percentage of abnormal DQ decreases.
F. All babies with weight > 2.5kg had normal Me, Mo DQ at 12 months.
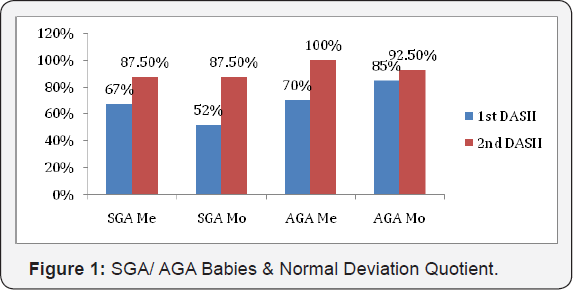
G. Small for Gestational Age (SGA)/ Appropriate for Gestational Age (AGA) & Deviation Quotients of DASII- (Figure1)
H. SGA babies were 75%. Abnormal DQ were more common
than in AGA babies. Improvement in DQ at 12months was more with AGA
babies than SGA babies (DQ improvement in SGA- Mo 87.5%, Me 87.5%, AGA
Mo 92.5%, Me 100%).
I. Gestational age & Deviation quotients of DASII-
J. 34wk (28%), 35 (34%), 36wk (38%). DQ improvement
more as gestational age advances. Improvement in MeDQ at 34 wks- 50%, 36
wks- 100%, MoDQ at 34 wks- 50%, 36 wks- 80%.
K. NNF risk factors & deviation Quotients-
L. Common Risk factors PROM (13 babies), Absent/
reversal EDF 8, Shock 3, Ventilation 3, hypoglycemia 3, Eclamsia 3,
Jaundice 3, multiple pregnancy 2.
M. 7 Babies continued abnormal DQs at 12m- reversal/
absent end diastolic flow, prolonged ventilation, IVH grade II- III, low
birth weight & PROM.
N. Improvement in Mental Outcome at 12 months- (Figure 2).
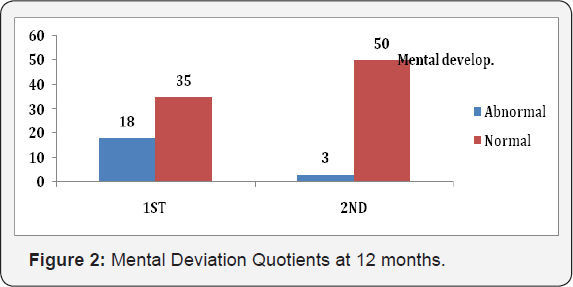
O.Out of 18 babies with abnormal MeDQ at 1st DASII, 16 babies normalized by 12 months.
P.94% babies had normal Me DQ at 12m.
Q. Improvement in Motor Outcome at 12 months- (Figure 3).
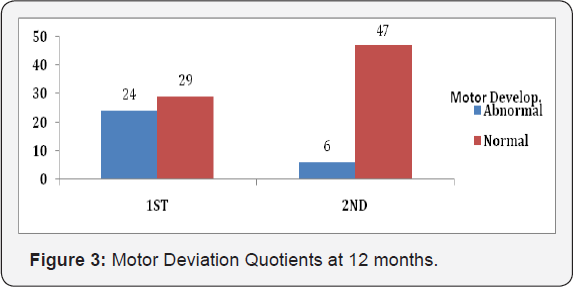
R.Out of 24 babies with abnormal MoDQ at 1st DASII, 20 Normalized by 12m.
S.89% babies had normal Mo DQ at 12m.
Discussion
Neurodevelopmental outcome in LP infants predominantly depends upon cause of prematurity, SGA/ AGA, associated risk factors [1,2,9]. High percentage of SGA babies was observed in our study, similar to findings of Lackman et al. [10].
With increasing birth weight & gestational age, Neuro developmental
outcome of LP infants improved in our study. The same was observed by
Schonhaut et al. & Carrie et al. [4,11].
7 Children who continued to have below average DQs at
12m were having severe risk factors. A similar observation was made by
Engle et al. [12].
Review of parent based Early Intervention RCTs show positive, clinical,
meaningful effects on cognitive and social development of LP infants [7,12,13].
CDC ES model starting from stimulation at NICU, lactation management,
multisensory stimulation, activities based on developmental milestones
has shown improvement in psychomotor functioning at one year, better
parent child bonding in at risk babies [8].
Conclusion
A. Early stimulation pivoting around parent-child in
LP babies has positive influence on Neurodevelopmental outcome at 12
months of corrected age.
B. Late preterm is a population at risk, to be monitored.
C. Association between NNF risk factors, primary
cause of prematurity and short term Neurodevelopment outcome in LP
infants need to address with larger sample size prospective study
Acknowledgement
Rajee Krishnan Ramkrishnan Unnithan, Developmental
Therapist, Lekshmi Madhavan Amritham,Preschool Teacher, CDC, Medical
College, Thiruvanathapuram.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment