The Role of Surgical Ligation of Patent Ductus Arteriosus in Very Preterm Infants: A Mini Review and Case Report-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Patent ductus arteriosus (PDA) in the very low
birth weight premature newborn (VLBWPN) is currently treated with
medical therapy or by surgical ligation. The objective of this
mini-review and brief case report is to highlight the potential side
effects of medical therapy (indomethacin or ibuprofen) including
bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC),
intraventricular hemorrhage (IVH), bowel perforation, pulmonary edema
and bleeding, retinopathy, thrombocytopenia, and decrease in renal
function and present an example of a patient frequently encountered in
the neonatal intensive care unit that dramatically improved with prompt
surgical intervention. Secondary objective is to support a more
proactive approach toward early surgical ligation and highlight factors
in VLBWPN who might be at the greatest risk and might benefit from
earlier intervention. Currently PDA ligation is generally performed in
the cases in which indomethacin or ibuprofen medication is unsuccessful
or contraindicated. Given the side effects of indomethacin or ibuprofen
medical therapy, it is important to recall the risks of nonoperative
management of VLBWPN and to consider earlier utilization of surgical
ligation.
Introduction
Patent ductus arteriosus (PDA) is a serious condition
frequently seen in the neonatal intensive care unit in premature
low-birth-weight infants. The reported incidence of PDA among premature
babies less than 28 weeks and 1000 grams is as high as 70%, and the rate
of spontaneous closure in very low birth weight premature newborns
(VLBWPN) is about 34% [1]. Patent ductus arteriosus (PDA) in preterm
infants is an important entity to diagnose since it is well established
to be associated with increased mortality and morbidities such as
bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), and
intraventricular hemorrhage (IVH); however, a causal relationship has
not been definitively established [2]. Patent ductus arteriosus, which
leads to significant hemodynamic, pulmonary, gastrointestinal,
cerebrovascular, and retinal problems, can be medically or surgically
treated; although, there has been an ongoing debate on which method
should be preferred [1]. However, studies show that PDA closure rates
with medical treatment are still low in VLBWPN. Failure of medical
intervention occurs in 40% to 50% of VLBWPN necessitating surgical
intervention [3,4]. In patients with a bleeding diathesis, necrotizing
enterocolitis (NEC) or where nonsteroidal anti-inflammatory drugs
(NSADs) are contraindicated surgical intervention is the only available
option [4]. Given the side effects of indomethacin or ibuprofen medical
therapy such as necrotizing enterocolitis, bowel perforation, pulmonary
edema and bleeding, retinopathy, thrombocytopenia, and decrease in renal
function [1] it is prudent to seriously consider an alternative to
nonoperative management of VLBWPN.
Case Report
Patient was a fourteen day old female born
premature at 24 weeks gestation. She was born via caesarian section due
to preterm premature rupture of membranes and fetal intolerance to labor
with a birthweight of 490 grams. She was noted to have Apgar scores of 5
and 8 and required immediate neonatal resuscitation with intubation for
respiratory distress syndrome (RDS). She subsequently was admitted to
the neonatal intensive care unit (NICU) for closer monitoring. At the
time of consultation, she was tolerating feeds and weighted 560 grams
but continued to require mechanical ventilation with inability to wean
Fi02 (upper 40%). A transthoracic ECHO cardiogram was performed in the
immediate postpartum period and found to be consistent with a large PDA
with left to right shunting.
The patient subsequently underwent attempted medical
therapy for closure of PDA with two courses of indomethacin.
Repeat transthoracic echocardiogram on day of life eleven was
found to be consistent with persistent moderate PDA with
continued left to right shunting with a gradient of 25-30mmHg
across the PDA. Other pertinent past medical history was
significant for questionable germinal matrix bleed, extreme
prematurity and respiratory failure. Other imaging included serial
daily chest x-rays consistent with RDS with bilateral fluid overload
that was unresponsive to Lasix.
Surgery was performed in the NICU; the patient was positioned
in the right lateral decubitus position and all pressure points
were padded. The left chest was prepped and draped. A posterior
lateral thoracotomy was performed with Bovie electrocautery just
inferior to the tip of the scapula and blunt dissection was preformed
down to the subcutaneous tissues; the latissimus dorsi muscle
was divided. The serratus muscle was then retracted anteriorly
and the third interspace was identified. The electrocautery was
further used to divide the intercostal muscles and the left chest
was entered. The aorta, recurrent laryngeal nerves, subclavian
artery, and the ductusarteriosus were identified; grossly normal
anatomy was noted. Dissection was then carried out inferiorly
and superiorly to the patent ductus arteriosus after the overlying
pleura was opened. A test clamp was then preformed which she
tolerated well. A medium clip was applied to the ductus, and it
was noted to occlude completely. The lung was reinflated and the
ribs reapproximated “with two 3-0 interrupted Vicryl sutures.
Likewise the muscles were reapproximated and finally the skin
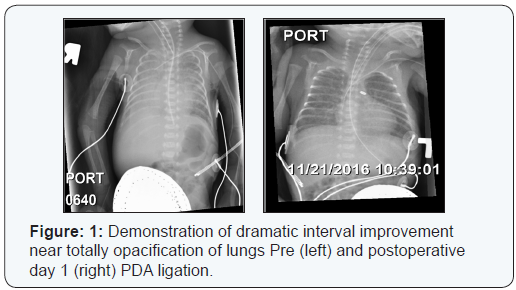
was closed in a subcuticular fashion. The postoperative chest
x-ray showed the clip in good position and the lungs adequately
reexpanded. The immediate postoperative course was uneventful
and the postoperative day one chest X-ray revealed dramatic
resolution of bilateral pulmonary infiltrates (Figure 1). The Fi02
was quickly weaned to the low 30s without difficulty. The neonate
resumed feedings on postoperative day one.
Discussion
Surgical PDA ligation is generally utilized after
medical
therapy with indomethacin or ibuprofen has been unsuccessful
at closure. Thoracotomy (eventually done bedside in the neonatal
unit to avoid transport) has been the standard of care for treating
large, symptomatic, or persistent PDAs since its inception in 1938 [3].
In a study by Trust et al, they found for infants under 800 g,
the failure rate for PDA closure with indomethacin was found to
be as high as 40%-50% [5]. In addition, indomethacin treatment
in VLBWPN has numerous severe side effects such as necrotizing
enterocolitis, bowel perforation, pulmonary edema and bleeding,
retinopathy, thrombocytopenia, and decrease in renal function [1].
Furthermore, other studies have clearly shown that the incidence
of NEC and the duration of TPN were significantly decreased in
premature infants with early surgical ligation of symptomatic PDA
that was refractory to medical treatment [6].
As highlighted by Weisz et al, it is important to note that
many of the observational studies on the treatment of PDA do
not adequately account for confounding by indication [7]. In
other words, it may be that PDA ligation is a surrogate marker
for increased illness severity, as “sicker” infants may be more
likely to be referred for ligation and therefore surgical ligation is
generally not considered until medical treatment has failed or was
contraindicated [7]. Studies to date have inadequately addressed
this confounding by indication.
The results from previous studies by Grosfeld et al and
Cassady et al support an opinion, that VLBWPN should undergo
early surgery as the treatment of choice [8,9]. The defined interval
from failed medical management in the VLBWN to surgical
ligation has not been defined and is likely multifactorial in nature.
Therefore, a brief period of conservative medical management
for VLBWN with PDA may be a reasonable approach, but without
rapid resolution and success with drugs, surgical closure of PDA,
generally assured and complete with one attempt, remains the
gold standard of treatment and should not be delayed.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment