Obstructive Fibrinous Tracheal Pseudomembrane: A Very Rare and Life-Threatening Complication of the Endotracheal Intubation-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Obstructive fibrinous tracheal pseudomembrane is a
rare complication associated with endotracheal intubation. We report the
case of a 10-year-old boy hospitalized for a severe abdominal trauma.
The boy remained intubated for 4 days. After extubation he started to
have stridor and acute respiratory distress so a reintubation was
necessary. After 24 hours, an elective extubation was performed and the
boy presented stridor and dyspnoea with no improvement with medical
treatment. A fibrinous mobile membrane was seen during a flexible
bronchoscopy. The pseudomembrane was removed and the patient remained
asymptomatic. The knowledge and an early diagnosis of this pathology is
very important due to be a life-threatening complication.
Introduction
Damage of the airways caused by intubation is usually
associated with mechanical trauma caused by the endotracheal tube
(ETT). Stridor occurs in approximately 1-16% of the patients, but in
4-8% of these children the extubation fails and an urgent reintubation
is needed. The most common causes are laryngeal or tracheal edema. The
symptoms are usually presented within 1-4 hours after extubation and are
usually resolved in under 24 hours. Stridor can persist in spite of the
treatment with nebulized epinephrine and steroidal therapy or with
repeated extubation failures. In such cases, a fiberoptic bronchoscopy
and differential diagnosis of common causes including subglottic
stenosis, vocal cord damage or subglottic/tracheal granulomas are all
required [1].
In recent years an infrequent cause of extubation
failure has been highlighted; obstructive fibrinous tracheal
pseudomembrane (OFTP) with a similar presentation of stridor
post-extubation. The knowledge of this pathology and its early diagnosis
is extremely important as this is a potentially life-threatening
complication [2].
Case Report
We present a case of a previously well 10-year-old
boy who was admitted to the Pediatric Intensive Care Unit after severe
abdominal trauma. The patient was under hemodynamic instability with an
hemorrhagic shock caused by an hepatic and pancreatic laceration. His
trachea was intubated with an appropriately sized 7-mm oral cuffed ETT,
that passed easily into the trachea. A caudal pancreatectomy was
performed. The child remained intubated and was on ventilatory support
for 5 days. The patient had no fever or suggestive signs of infection in
repeated blood testing. The blood culture and tracheal aspirates were
negative. The chest x-ray was normal. A few hours after the extubation,
the boy started to have severe stridor and acute respiratory distress
and a reintubation was necessary. There were no early complications with
the reintubation and the patient improved immediately. Repeated ETT
suction revealed no secretions. After 24 hours, an elective extubation
was performed. Inspiratory stridor and dyspnea started shortly after
extubation with normal SpO2. The cause of the respiratory distress was
thought to be laryngeal edema and this was treated with inhaled
budesonide and intravenous steroidswith no improvement.
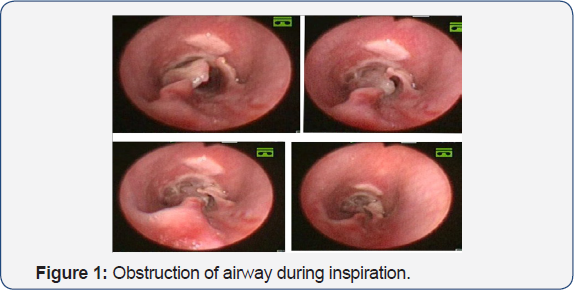
The symptoms became progressively worse and blood gas
results showed increased PCO2, so a flexible bronchoscopy was
performed. In the trachea, a white, fibrinous mobile membrane was seen
two centimeters below the subglottis in an anteroposterior and
transverse position. This caused an intermittent complete obstruction of
the airway during the inspiration (Figure 1). A rigid bronchoscope was introduced and the pseudomembrane was introduced and the pseudomembrane was removed.
The patient remained asymptomatic after extubation
without difficulty breathing or stridor. The control bronchoscopy showed
a normal airway size with a mild erythematous circumferential area.
Secretions or other inflammatory symptoms were not observed. 21 days
after admission the child was discharged home asymptomatic with no
further complications.
Discussion
OFTP is a very rare and life-threatening complication of the endotracheal intubation. The first case was described in 1999 [2].
Birch described the first pediatric case in the year 2005. A 8-year-old
that developed stridor in the first 24 hours after extubation for
dental surgery with general anesthesia [3].
The real incidence is unknown as endoscopy to review airway injury
after intubation is not a routine process. In 2011 a short series was
reported in which a total of 24 adult patients were described and a
review of the literature was made[4].
It is usually not considered a complication after a bronchoscopy in
Pediatric Intensive Care Unit (PICU) patients or in Neonatal Intensive
Care Unit (NICU) patients. However, a recent retrospective study
performed over a 10 year period describes OFTP in 1.4% of PICU or NICU
patients who had symptoms or clinical signs after extubation [1].
The hypothesis is that the pseudomembrane formation is caused by an
ischemic injury of the tracheal mucosa and submucosa, which causes
ulceration and necrosis. Finally, a fibrinous exudate and an
infiltration of polymorphonuclear neutrophils can be observed, causing a
functional stenosis [5].
The tracheal ischemia due to cuff pressure injury of the ETT has been
suggested as the etiology, nevertheless it has been reported in children
intubated with no tracheal cuff [1,3].
It is also associated with traumatic intubation or inappropriately
large ETT. The OFTP can occur in patients within a short time of
intubation; however the average time of previous intubation is 37 hours.
The clinical presentation consists of stridor and a different grade of
dyspnea that typically occurs before 24 hours postextubation in the
pediatric patients. In adults this can occur 10-15 days later [4].
An important difference between OFTP and laryngeal edema is that OFTP
does not respond to medical treatment. Differential diagnosis includes
staphylococcal tracheobronchitis with tracheal pseudomembranes. In these
cases, cultures could be positive, sepsis could be a clinical
presentation and the lesion might not necessarily be localized to the
site of the cuff or in the subglottis area. Bronchoscopy is used to
diagnose OFTP. The typical endoscopic findings are circumferential
membranes firmly attached to the trachea that move (or not) in the
airway with the respiratory cycle. It can collapse the airway
completely. It can be an annular or flapping septum. The lesion is
located in the subglottis and the first tracheal rings. The rest of the
airway is normal. Standard treatment includes rigid bronchoscopy and
removal of the tracheal membranes. However, a flexible bronchoscopy with
forceps or mechanical removal with a tracheal balloon can also be
useful. There is no sequela. In some cases described in adults the
condition fully resolved after expectoration with spontaneous membrane
removal [5].
Conclusion
In conclusion, in patients with clinical symptoms of
stridor and dyspnea after extubation that does not improve with medical
treatment it is important to think about the formation of a tracheal
pseudomembrane that causes airway obstruction. This obstruction can be
intermittent or positional and can be life-threatening. Pediatric
pneumologists, intensivists and otorhinolaryngologists should know this
pathology for early bronchoscopic diagnosis and treatment.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment