Diagnosis and Treatment of Supraventricular Tachyarrhythmia in Pediatric Population: a Review Article-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Supraventricular tachyarrhythmia (SVT) is the most
common tachyarrhythmia in pediatric patients and accounts for more than
90% of pediatric arrhythmias. As many as 16 different mechanisms of
pediatric SVT exist; we focused in this review article on the three most
common groups of SVT mechanisms in pediatrics: atrioventricular
re-entry tachyarrhythmia (AVRT), atrioventricular nodal re-entry
tachyarrhythmia (AVNRT), and a trial tachyarrhythmia (AT). Many methods
have been implicated in the diagnosis of SVT like full history taking
regarding onset and frequency of palpitation, syncope, chest pain,
dispend, heart failure, drug intake and physical examination. Children
with suspected SVT must be subjected to resting 12-lead surface ECG and
ECG during the attack. Echocardiography must be done for detection of
any structural heart diseases. Moreover, recent techniques like Electro
physiologic study (EPS) is the most definitive diagnostic procedure.
Many therapeutic strategies like drugs and radiofrequency ablation (RFA)
have been succeeded to provide a significant reduction of the risk of
SVT, but RFA offers the prospect of cure of the arrhythmia and avoidance
of drug-associated side effects. It is often becoming the first line of
therapy for many children with SVT, as it has a relatively low
morbidity and mortality, and it results in a low rate of recurrence of
SVT.
Keywords: SVT; Children; Diagnosis; Treatment
Core Tip:
This manuscript discusses the most common types, recent strategies in
diagnosis and management of Supraventricular tachycardia in pediatric
age group.
Introduction
Supraventricular tachyarrhythmia (SVT) is the most
symptomatic pediatric arrhythmia resulting from an abnormal mechanism
that requires structures in the heart above the bifurcation of the
bundle of His for its continuation. Clinical symptoms of SVT are
variable; ranging from asymptomatic or minor palpitations to more severe
manifestations [1]. Theincidence of SVT has been documented to affect between 1 in 250to 1 in 25,000 children [2].
Variable mechanisms ofSVT exist; we concentrated on
the three commonest forms occurring in children which are:
atrioventricular re-entry tachyarrhythmia (AVRT), atrioventricular nodal
re-entry tachyarrhythmia (AVNRT), and a trial tachyarrhythmia (AT) [3].
Most Common Types of Svt in Pediatrics
Atrioventricular re-entrant tachyarrhythmia (AVRT) or accessory pathway re-entry tachyarrhythmia.
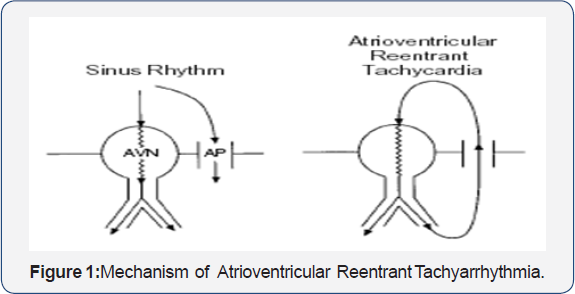
An accessory pathway (AP) is a microscopic bridge of
muscle connecting atrium and ventricle that bypasses the normal
electrical insulation of the AV ring. The impulse spreads down either
via the atrioventricular (AV) node or the AP and then up the other A
re-entrant unconventional circuit is formed, [4] (Figure 1).
AVRT is the commonest type of SVT in the pediatric
population forming two-thirds of the affected children, then comes the
atrioventricular nodal reentry tachyarrhythmia (AVNRT) and the trial
tachyarrhythmia (AT) [5].
AVRT is more common in males, but its incidence decreases with age. On
the other hand, the incidence of AVNRT and a trial tachyarrhythmia is
increased with age [6].
Atrioventricular nodal reentry tachyarrhythmia (AVNRT)
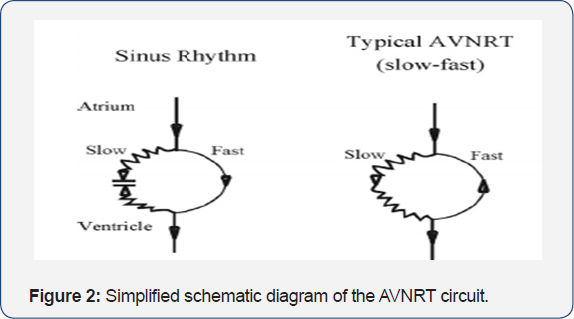
The AV node is composed of "slow" pathway and "fast"
pathway. AVNRT happens when an ante grade impulse is blocked at one
pathway (usually the fast pathway), resulting in conduction over the
other (usually the slow pathway). After the impulse is travelled down
via the slow pathway, the fast pathway is now unblocked and the impulse
can spread retrograde via the fast pathway. So, a re-entrant circuit is
formed, [7] (Figure 2).
AVNRT accounts for 15% of cases of pediatric SVT,
mostly present over the age of 5 years and almost completely absent in
infants. Females were more than males in cases diagnosed as AVNRT or AT [6].
Atria tachyarrhythmia (AT). AT is mostly due to abnormal automaticity,
may be formed by remnant embryonic cells with automatic qualities,
causing abnormal impulses that come away from normal sinus node but
still within the atria. Although it is a rare condition, but still the
third common mechanism of tachyarrhythmia occurring in children, if
remains undetected can result in a dilated cardiomyopathy [7].
History and clinical presentations of Svt in pediatrics
The clinical presentation varies with the age of the
patient; generally, it differs in infancy from that in an older child.
In infancy most attacks occur before 6 months of age, and may often less
than 4 months. They may be undetected or associated with pallor The
parents may take their child to the doctor with a complaint of poor
feeding, or vomiting. The rapid breathing or ashen color may not be
observed by them. By the time, the pediatrician sees them: there is
usually significant cardio-respiratory distress. The infant will often
have signs of heart failure. Occasionally frank circulatory shock will
be present [8].
Occasionally, a young patient may have palpitations, chest or abdominal
pain, occasionally syncope, particularly with exertion may occur, but
the presence of congestive heart failure beyond infancy is extremely
uncommon [9](Table 1).
Physical Examination of Svy in Pediatrics
Following the history, the physical examination
should be performed: unexplained hypothermia, with poor perfusion, a
picture of sepsis but with negative cultures. In the older infants,
irritability associated with vomiting and sometimes diarrhea (uncommon).
In approximately 20% of infants, SVT is detected during the routine
examination without symptoms [10].
Auscultation should be done to reveal the presence of
structural heart disease, heart rate and rhythm should be noted.
Further evaluation will depend on the severity and frequency of
symptoms, the age of the child, and the presence of structural heart
disease. Infants with SVT may have a heart rate range from 220 to 300
BPM. Older children generally have slower rates which may count from 180
to 240 Bpm. Untreated SVT can result in congestive heart failure (CHF)
within 24 to 48 hours. Termination of the attack by vagal maneuvers may
suggest a reentrant tachyarrhythmia involving AV node [5].
Diagnostic investigations of Svt in pediatrics
Recording a 12- Lead Electrocardiography (ECG) at
rest should be done and examined for any abnormal rhythm, delta waves,
abnormal QT interval, sinus tachyarrhythmia, or any sign of underlying
structural heart disease. [11].
ECG can clearly diagnose about 80% of AVNRT and AVRT, but incorrectly
categorize approximately 20% of cases of SVT; therefore, the ECG cannot
serve as the sole means for determining the mechanism of tachyarrhythmia
[12].
Another diagnostic tool is worn by the patient named
Holter monitor. It can record continuous ECG tracing for 24 to 48
hours,having the same idea as classic ECG wires and electrodes but it is
a portable device that provides information about symptoms that can
occur during the day [7].
In selected patients with occasional complaints (i.e.
less than two episodes of SVT per month) and associated with disabling
symptoms (i.e. hemodynamic instability) can be diagnosed by implantable
loop recorders. If the clinical history is not enough or other measures
have failed to identify the SVT mechanism, then recordings and
stimulation can be done via Tran esophageal a trial loops for these
patients for diagnosis or to provoke paroxysmal tachyarrhythmia [13].
The possibility of structural heart disease should be
excluded by Echocardiography examination in children with identified
attacks of SVT, which is not possible to be detected via physical
examination or resting 12-lead ECG [14].
Other investigations can be done to exclude other
causes included in the differential diagnosis of SVT Chest x-ray with
lateral and anteroposterior views is done to diagnose cardiomyopathy and
CHF. Laboratory tests which include; serum electrolytes to diagnose any
imbalance leading to abnormal cardiac rhythm, complete blood cell count
(CBC) with differential to exclude infections or anemia, also,
screening of toxic substances, thyroid function tests, and arterial
blood gas can be helpful [5].
The most accurate diagnosis can be done with the
electrophysiological study (EPS). It is used for clear classification of
different mechanisms of SVT Also, EPS combined with catheter ablation
can be used as a definitive long-term therapy [7].
Management of Svt in Pediatric Age Group
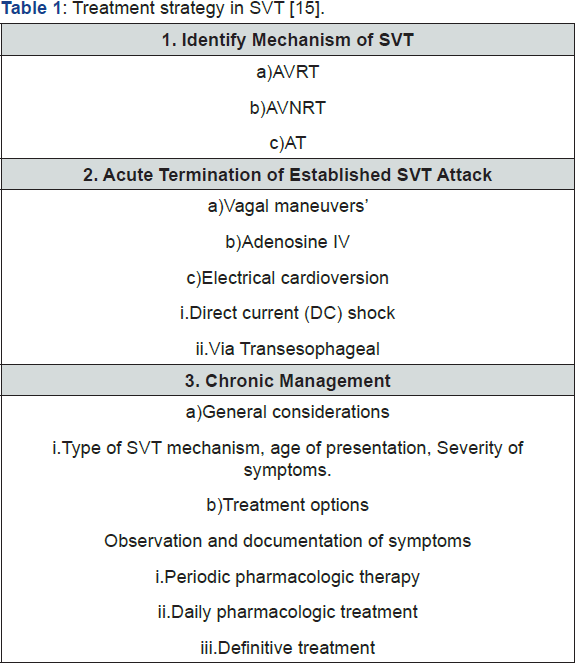
The dealing with SVT can be done in two ways: acute
termination of the attack of tachyarrhythmia and prevention of
recurrences (chronic therapy). The acute treatment begins with
documentation of the arrhythmia with a 12 lead ECG, assessment of
hemodynamic status and recognition of the arrhythmia mechanism. Chronic
therapy is based on the SVT mechanism, the patient's age, and the
frequency and patient's complaint during the attack as well as access to
medical care and sophistication of the patient caretaker (Table) [15].
Acute management of Supraventricular tachyarrhythmia
For the aerodynamically tolerated episode, vagal
physical maneuvers are to be used first. The patient may be taught to do
Valsalva maneuver (the most potent physical maneuver), induce vomiting,
dive the face in the iced water for 10-20 seconds, or carotid sinus
massage may be done, an ocular pressure is not recommended for children.
These physical maneuvers are potent in terminating re-entry SVT; mostly
AVRT and to less extent AVNRT [11].
An ultra-short-acting drug (Adenosine) is highly
effective in terminating AV node-dependent SVT, but it is of limited
value in the diagnosis of AT. Vagal maneuvers and adenosine produce
transient AV node block and result in sudden termination of SVT in any
tachyarrhythmia involving AV node but not in AT [16].
The use of Beta blockers or long-acting calcium
channel blockers is of value especially for patients with frequent a
trial or ventricular premature beats which may act as a cause of
recurrence of SVT but they must be used with great caution as they may
potentiate hypotension [11].
In an aerodynamically unstable child with severe
hypotension, electrical cardio version by synchronized DC shocks is the
treatment of choice. It is a safe and effective procedure in the
majority of patients [2].
Long term (chronic) management of Supraventricular tachyarrhythmia
The decision to initiate chronic therapy in infants
and children is based on symptoms, efficacy rates, safety issues,
expected response to therapy and frequency of episodes. The range of
therapeutic options aimed at treating disorders of heart rhythm has
expanded tremendously over the past decade; the complexity of actions
produced by ant arrhythmic agents occasionally leaves the clinician
frustrated by attempted at predicting the clinical results [2].
A child with SVT should be viewed globally while
putting a long-term therapeutic plan, as this may affect him through his
lifelong. A pharmacologic therapy is used to provide symptom relief.
The usual selection of drugs (in order) is propranolol, verapamil and
amiodarone. Dioxin is especially considered in cases with AVNRT, while
amiodarone in combination with propranolol or/ and verapamil is
effective in cases with AT [11].
Radiofrequency ablation (RFA) using the traditional
radiofrequency energy to heat and destruct the site of origin of the SVT
mechanism has been more widely applied in children since the 1990s [3].
It is now considered as the first line of management for many children
with SVT and offering the prospect of cure of the arrhythmia and
avoidance of drug-associated side effects. Success rates for ablation
are as high 95% and characterized by low morbidity, low mortality, and a
low rate of SVT recurrence [17]
. RFA may have some complications resulting from the vascular access
(i.e. hematomas, perforation of the aorta, deep venous thrombosis), or
during catheter manipulation (i.e. alular damage, perforation of the
coronary sinus or myocardial wall), or inaccurate ablation (resulting in
i.e. AV node block, myocardial perforation, coronary artery spasm,
transient ischemic attacks)[18]
. Successful elimination of SVT substrate results in improving the
pediatric quality of life regarding physical, emotional, social, school
and psychosocial functions [19].
In conclusion, SVT is a common pediatric age group
problem. Many methods have been implicated in the diagnosis of SVT like
detailed history taking and physical examination. ECG and
echocardiography must be done to children suspected to have SVT Electro
physiologic study (EPS) is a recent technique for definitive diagnosis.
RFA is a definitive therapy for many children with SVT However, further
studies are mandatory in order to provide more novel therapeutic agents
for complete protection of SVT and decreasing the complications of
already used management procedures.
Acknowledgement
The author is grateful for Deanship of Scientific Research (DSR), Taibah University and Medina, Saudi Arabia for support.
Author Contributions
Abo Hadeed H.M.A. did the literature review and
analysis, wrote the paper; drafting and critical revision and editing,
and final approval of the final version.
Open-Access
This article is an open-access article which was
selected by an in-house editor and fully peer-reviewed by external
reviewers. It is distributed in accordance with the Creative Commons
Attribution Non Commercial (CC BY-NC 4.0) license, which permits others
to distribute, remix, adapt, build upon this work non-commercially, and
license their derivative works on different terms, provided the original
work is properly cited and The use is non-commercial. See:
http://creativecommons.org/ licenses/by-nc/4.0/
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment