Traumatic Pancreatitis in Children-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Traumatic pancreatitis is still a relative
enigma, despite modern clinical practice, technology and modern
diagnostic procedures. This condition is very specific and serious and
is associated with significant morbidity, especially in pediatric
population. Traumatic pancreatitis is also an emerging problem in
pediatric population with its incidence rising in the last 20 years.
Data regarding the optimal management and physician practice patterns
are lacking. We present a literature review and updates on the
management of pediatric pancreatitis due to trauma. Prospective
multicenter studies are necessary to guide care and improve outcomes for
this population.
Keywords: Trauma; Pancreas; Children; Diagnosis; ManagementIntroduction
Traumatic pancreatitis is still a relative enigma,
despite modern clinical practice, technology and modern diagnostic
procedures. This condition is very specific and serious and is
associated with significant morbidity, especially in pediatric
population.
Pancreatic injury is the fourth most common abdominal
organ injury (following injuries of the spleen, liver and kidneys) [1].
Pancreatic injuries are usually very hard to identify by different
diagnostic imaging methods, and these injuries are often overlooked in
patients with multiorgan trauma [2]. Unfortunately, in literature, our
current understanding and approach to the management of traumatic
pancreatitis in children is still based on studies in adult population.
In this article, we will try to summarise current knowledge about
traumatic pancreatitis in children and recommended diagnostic and
therapeutic procedures.
Etiology and Epidemiology
Pancreatic trauma is divided into non-penetrating
(blunt) and penetrating injuries. In children, the most common type of
trauma mechanism is blunt trauma (motor vehicle crashes, falls, violence
and they are typically seen after crashes involving a bicycle
handlebar) [3-5]. There is two typical scenarios: isolated injury caused
by a direct blow to the upper abdomen and multisystem trauma caused by
high-energy mechanisms (usually avulsion of the blood supply by rapid
deceleration, puncture by a fractured rib, or crushing against the
vertebral column) [6,7].
Isolated pancreatic trauma occurs in penetrating
injuries due to anatomic position of pancreas. Pancreatic trauma occurs
in 3% to 12% of blunt injuries, and 1,1% of penetrating injuries in
children [8]. According to the American Association for the Surgery of
Trauma, the guidelines for pancreatic injuries are:
- Grade I: minor contusion without duct injury or superficial laceration;
- Grade II: major contusion or laceration without duct injury or tissue loss;
- Grade III: distal transection or parenchymal injury with duct injury;
- Grade IV: proximal transection or parenchymal injury involving the ampulla;
- Grade V: massive disruption of the pancreatic head [1].
Onset of acute pancreatitis is one of the most serious complications of traumatic injuries.
According to etiology, trauma is the cause of acute pancreatitis in 7,6% to 36,3% [9].
According to literatures, blunt abdominal injuries occur in 10-15% of injured children [10].
Abdominal trauma is the cause of acute pancreatitis in 23% [11].
Suzuki reported that trauma is cause of pancreatitis, even in 36% [9].
Anatomy and Phisiology
Pancreas is an abdominal organ, relatively protected
by ribs. The rib cage provides a bone structural protection. This
protection is less effective during childhood because the ribs in
children are
elastic. In addition, children have relatively larger viscera, less
overlying fat, and weaker abdominal musculature. The pancreas
grows rapidly during first five years of life and after that period
the growth slows down up to the age of 18 years [10].
It is a large complex gland which lies outside the walls of the
digestive tract, parallel to the stomach at the level of the first and
second lumbar vertebrae. The upper abdominal intraperitoneal
organs are situated at the front and paraspinal muscles situated
at the back. The lobules of the pancreas drain into the main
pancreatic duct of Wirsung along the entire gland and joins the
common bile duct, emptying into the duodenum through the
ampulla of Vater [9,12].
Pancreas is not capsuled, so pancreatic enzymes could be
found in the peritoneal cavity. Normally, healthy pancreatic
acinar cells, lysosomes, containing cathepsin B, which is involved
in intracellular and extracellular digestion. Zymogene granules
containing digestive proenzymes (trypsinogen) are released,
and these proenzymes remain inactivated [9]. Even if trypsin is
activated in the pancreas for some reasons, its activity is blocked
by pancreatic secretory trypsin inhibitor. If trypsin leaks into
the blood, the endogenous trypsin inhibitors α1-antitrypsin
and α2 macroglobulin bind to trypsin and suppress its activity.
The sphincter of Oddi prevents reflux of duodenal fluid into the
pancreatic duct [9,13].
Pathophisiology
Pancreatitis is a complex multifactorial disease and more
than one etiological factor may be identified as its cause [14].
Pancreatitis which is the result of trauma may be extended to the
peripancreatic tissues and remote organs [15].
Excessive stimulation of pancreatic exocrine secretion can
cause reflux of pancreatic juices and enterokinase, pancreatic
duct obstruction, and inflammation. These conditions can disrupt
defence mechanisms, activate trypsin beyond the level of trypsin
inactivation, and increase attacking factors leading to acute
pancreatitis [9,15,16]. The activation of zymogene protease in
pancreatic acinar cells plays an important role in the development
of acute pancreatitis [9].
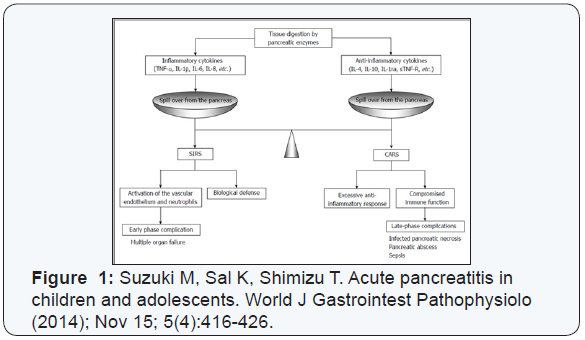
In severe pancreatitis, vasoactive substances such as histamine
and bradykinin are produced in large amounts with trypsin
activation. Because of that, third spacing of fluids and shock due to
hypovolemia may occur. In addition, leakage of activated enzymes
from the pancreas causes secondary cytokine production. These
cytokines trigger the systemic inflammatory response syndrome
(SIRS) [9]. SIRS results in hyper activation of macrophages and
neutrophils, and release tissue injury mediators. In that case we
can expect multi-organ failure and respiratory distress syndrome
[9].
As a biological defence response, anti-inflammatory cytokines
and cytokines antagonists can prevent prolongation of SIRS. This
predominance of antagonists of cytokines is called compensatory anti-inflammatory response syndrome (CARS) [9,17]. CARS
inhibits the production of new cytokines, infection of vital organs
can occur, and as a results of the infection, endotoxins in the blood
stimulate neutrophil aggregation in distal organs, tissue injury
mediators are released, and distal organ failure occurs [9] (Figure
1).
Diagnosis
Pancreas injuries are usually difficult to recognise due to
retroperitoneal position of the organ, and pancreas injuries are
usually not isolated. The diagnosis of acute traumatic pancreatitis
should be kept in mind after every blunt abdominal trauma in
children! Typical trias symptoms in acute pancreatitis in children
are: pain, leukocytosis and elevated levels of serum amylase.
Clinical symptoms
Abdominal pain is an important early symptom in children.
In older children, the frequency of abdominal pain is similar to
the one in adults, whereas in younger children vomiting is an
important clinical symptom [9,16]. Other symptoms are: jaundice,
fever, diarrhoea, back pain etc. A child may have bruises, such as a
handlebar mark on the abdomen, or may not have any marks at all.
Imaging
A plain X-ray of the abdomen in patients with pancreatic
trauma is nonspecific, but it is valuable in prediction of severity.
Conventional radiography can be valuable in detecting penetrating
trauma [2,6,9]. Ultrasonography is a convenient and non-invasive
test. An ultrasound is usually performed to enable the diagnosis
of free abdominal fluid or gross damage to the liver or spleen. The
pancreas is not easy to identified, so pancreatic injuries can be
missed [6,18]. However, it is a very useful method of diagnosis and
evaluation of complications.
CT scans provide the best overall method of diagnosis and
recognition of a pancreatic injury [19]. MRCP (magnetic resonance
cholangiopancreatography) is a non-invasive procedure for
diagnosis of the integrity of pancreatic duct with high sensitivity
and specificity. MRCP is also very useful in searching for cause of
acute pancreatitis in children [2,6,9].
ERCP (endoscopic retrograde cholangiopancreatography)
was reported as very useful diagnostic method for pancreatic
duct injury, and it also can be a definitive test to demonstrate the
location of duct disruption and the grade of disruption. Also, ERCP
is an effective and safe non-operative treatment tool [6].
Laboratory investigations
Laboratory investigations are usually non-invasive and nonspecific
as a diagnostic method for traumatic pancreatitis. Raised
level of amylase in serum can be useful in diagnosis, but there is
poor correlation between raised amylase and pancreatic trauma,
because amylase may also be elevated in injuries of the salivary
gland, in duodenal trauma, hepatic trauma, injuries of head and
face [2]. A raised amylase level after blunt trauma of pancreas
is time dependent, and a persistent elevation is an indicator of
pancreatic trauma, but it does not indicate the severity of the
injury [2]. Low disease specificity is a problem [9].
Activity of serum lipase is also not specific of pancreatic injury
[9]. The problem is a low disease specificity (sensitivity is 86,5-
100% and specificity of 84,7%-99,0% for diagnosing pancreatitis).
Its sensitivity is higher in comparison to serum amylase 99). In
severe pancreatitis, serum lipase level is seven times higher than
normal within 24 hours after onset of pancreatitis [20].
Serum amylase has a shorter half-life and rises earlier than
serum lipase. Other pancreatic enzymes have also been described
as markers of inflammation, including carboxyl ester lipase,
isoamylase and phospolipase-A2 [21]. Other laboratory tests
include: glucose, calcium, triglycerides, transaminases, bilirubins,
white blood cells, urea nitrogen and serum albumin [21].
Therapy
Depending on the grade of the pancreatic injury, available
therapies are surgical or conservative. The initial treatment of
pancreatitis is to withhold oral intake of food and fluid, to prevent
stimulation of pancreatic exocrine secretion. The main goal of
therapy is to be supportive! That includes adequate rehydration,
analgesia, pancreatic rest, restoration of normal metabolic
homeostasis [18].
Pain management
There are no data about which analgesic is optimal for
children with acute pancreatitis. Morphine or related opioids
were used in 94% of children with acute pancreatitis [22]. Despite
concerns that morphine may cause sphincter of Oddi spasm and
thus exacerbate pancreatitis, there are limited and opposing data.
Cochran’s analyses do not support this opinion, but the study was
limited to a small number of children [23].
Hebra suggested that acetaminophen, as a peripherally acting
drug, is the choice for mild pain and elevation of body temperature;
tramadol, as a centrally acting analgesic, is used for moderately
severe pain; meperidine, as a synthetic opioid narcotic analgesic,
is used for severe pain [18]. According to Abu-El Haija et al., newer
medications, including intravenous acetaminophen and ketorolac,
reduce narcotic use in paediatric acute pancreatitis [21]. Suzuki et
al. state that pentazocine, metamizol and morphine are commonly
used medicaments [9].
Intravenous fluid management
Because fluid leaks into the surrounding tissue due to
inflammation associated with acute pancreatitis, adequate
infusion to supplement extracellular fluid is needed during initial
treatment. In severe cases, increased vascular permeability
and decreased colloid osmotic pressure causes extravasation
of extracellular fluids into the surrounding tissue and
retroperitoneum and, later, into the peritoneal and pleural cavity
leading to large loses in circulating plasma volume [24].
We still don’t know which fluid and what volume are optimal
in children. The results of a small study conducted a few years ago
support aggressive approach in fluid therapy [25]. However, the
data obtained in another study reported that excessive hydration
(10-15ml/kg/h) resulted in increased organ failure, respiratory
insufficiency and mortality [24-26].
Most commonly, crystalloid solutions are the choice for
resuscitation [21,27]. Recently, a randomised controlled trial
on the use of lactated Ringer’s solution versus normal saline
(although in adults) found that there is a reduction in the
systemic inflammatory response syndrome in lactated Ringer’s
solution[21,28]. All paediatric patients during intravenous fluid
resuscitation have to have good hemodynamic monitoring.
Antibiotics
Antibiotics are not recommended in all cases of children with
traumatic pancreatitis. In mild cases of pancreatitis the incidence
of infectious complication is low, and prophylactic antibiotics
are not necessary. However, antibiotics should be considered if
severity increases or complications develop. Antibiotics should be
selected so that there is a good tissue distribution to the pancreas
[9].
Hebra et al., suggested using ampicillin, ceftriaxone, imipenem
and cilastatin [18]. A recent meta-analysis from 2015, which
included high-quality trials with prescription of prophylactic
antibiotics within 2 days after hospital admission and within 3
days of onset of the pain, demonstrated a significant reduction of
mortality (7,4% vs. 14%) [29].
Nutritional support
There are no published data in paediatric patients concerning
optimal time for starting nutrition and the type of nutrition which
is optimal in children with traumatic pancreatitis. Children with
acute pancreatitis are at risk of acute malnutrition due to two
conditions: the first is the increase in energy intake ant nutrient
requirements related to their catabolic disease and the second is
iatrogenic or spontaneous oral food restriction. The nutritional
risk is inversely proportional to the age as growth speed and
energy/ nutrient requirements are higher in younger children
[16].
According to recent meta-analyses, enteral nutrition
was
superior to total parenteral nutrition with a lower incidence of
infection and multi-organ failure, resulting in lower mortality rates
and a shorter hospital stay [21,30]. Enteral nutrition prevents
the systemic inflammatory response, luminal stasis, bacterial
overgrowth and bacterial translocation [16]. Enteral nutrition
is superior in children with traumatic pancreatitis because it
prevents acute malnutrition, provides better intake of nutrients
for healing the tissue, modulates systemic inflammatory response
and thus prevents multiple organ failure [16]. Li and co-authors
suggested that early enteral nutrition (within first 48 hours) is
very important [31].
Early enteral feeding should be via nasojejunal tube to avoid
secretion of cholecystokinin, secretin and pancreozymin, and also
pancreatic exocrine function will be on minimum. There is no
difference in the outcomes of polymeric and elemental formulas
and there is no evidence that immune enhancing nutrients or
probiotics are helpful in the management of pancreatitis. Optimal
nutritional therapy in paediatrics should be studied further so
that it can be uniformly applied [21].
Elementary diet formula or formula with oligopeptides seems
to be the best option for maximal suppression of pancreatic
secretion. For these reasons, we can concluded that the most
important are nasojejunal feeding tube, elemental formula and
24-hours continuous enteral infusion [16].
Surgical management
Grade III and higher grade pancreatic trauma need operative
management (resection or possible reconstruction and/or
drainage). However, a recent study shows some controversy and
considers a non-operative management of high-grade pancreatic
trauma [32].
Conclusion
Traumatic pancreatitis is an increasingly recognised clinical
entity which may be the result of improved recognition. Children
are not small adults, and pancreatitis in this population is different
from the one in adults in their etiology, clinical manifestation,
severity and outcome. Well designed prospective studies are
needed in all areas of diagnostics and management of paediatric
traumatic pancreatitis.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment