Sensitivity Pattern of Micro Organisms of Septicemia in Neonatal Intensive Care Unit of a Tertiary Hospital, Bangladesh-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Neonatal septicemia is a clinical syndrome of
systemic illness accompanied by bacteremia occurring in the first 28
days of life. Micro-organism causing neonatal septicemia varies from
country to country and region to region and time to time. In many
situations, conventional antibiotics are not sensitive to causative
micro-organism. Our aim of the study is to identify causative organism
and sensitivity pattern of micro-organism in Neonatal Intensive Care
Unit, (NICU)
Methods & Subject:Total 300
patients were enrolled in this study with clinically diagnosed
septicemia with prior antibiotic treatment or not. This study was done
in NICU of tertiary Hospital, Chittagong Medical College, Bangladesh
during the period of January 2013 to July 2014. Blood culture was done
in Bact/Alerd 3D system.
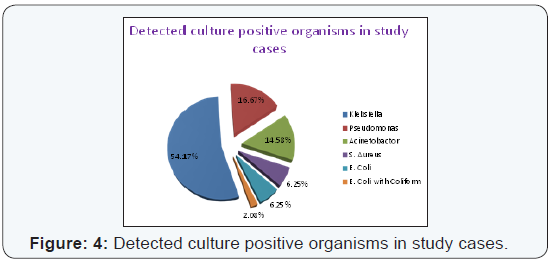
Result: Out of 300 cases, 204 cases
were culture negative and 96 cases (32%) were culture positive.
Klebsiella is the commonest causative organism 52(54.17%), followed by
Pseudomonas 16(16.67%), Acinetobacter 14(14.58%), S. aureus 6(6.25%),
E.coli 6(6.25%), E. coli with other Coliform 2(2.08%). In this study,
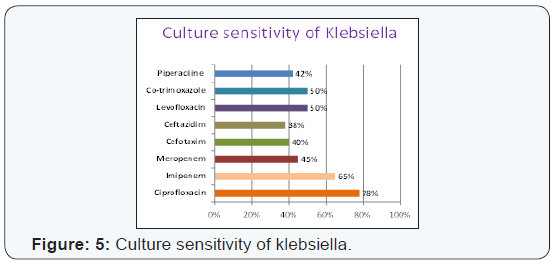
sensitivity of Klebsiella was mostly to Ciprofloxacin, Imipenem,
Azithromycin, Co-trimoxazole, Piperaciline and Tazobactam. Sensitivity
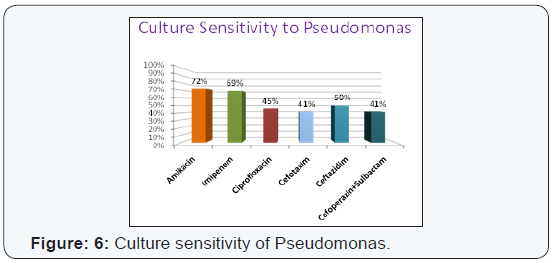
to Pseudomonas was mostly to Amikacin, Imipenem, Ciprofloxacin,
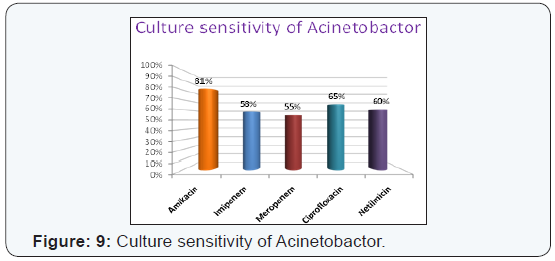
Azithromycin and Cefoperazone with Sulbactum.. Sensitivity to
Acinetobactor was mostly to Amikacin, Imipenem, Ciprofloxacin,
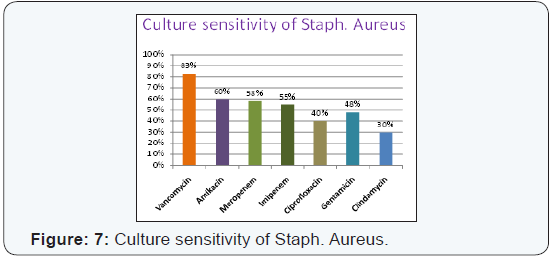
Netilmicin. Sensitivity to S. aureus was mostly to Vancomycine,
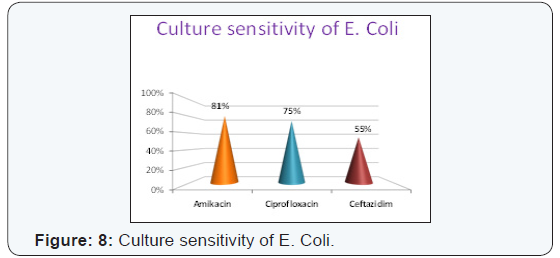
Amikacin, Imipenem, Meropenem.. Sensitivity of E.coli was mostly to
Amikacin, Ciprofloxacin, Ceftazidin. Most of the culture positive
organisms not sensitive to conventional Ampicilin, Gentamycin.
Conclusion: Microorganisms
identified causing neonatal septicemia in our region are Klebsiella,
Pseudomonas, Acinetobactor, E. coli and Enterobector. Antibiotic
sensitive to identified microorganism were Amikacin, Ciprofloxacin,
Levofloxacin, Imipenem, Meropenem, Vancomycin and
Ceftazidim..Conventional Ampicillin sensitivity is not detected and
Gentamicin sensitivity is also low.
Keywords:Zinc; Malnutrition; Renal failure; BoneIntroduction
Neonatal septicemia is a clinical syndrome of
systemic illness accompanied by bacteremia occurring in the first 28
days of life [1]. Micro-organisms causing neonatal septicemia are a bit
different from region to region and also country to country depending
upon various factors especially socioeconomic conditions and personal
hygiene with environment. It may occur through transplacental infection
or an ascending infection from mother’s genitourinary tract and from the
infected caregiver or nosocomial infections. The incidence of neonatal
sepsis is 5 to 8 per 1000 birth, the highest rates occur in LBW,
perinatal asphyxia, maternal infection and babies with congenital
abnormalities [2]. In global perspective microorganisms most commonly
associated with neonatal sepsis include groupB Streptococci,
coagulase-Negative Staphylococci, Klebsiella, and Pseudomonas,
Enterobacter, Candida, Streptococcus, anaerobes and non typeable H
influnzae. It is important to note that 20-30% of the survivors of
neonatal sepsis may exhibit neurological sequelae [2]. Sepsis
related mortality is however largely preventable with rational
antimicrobial therapy and aggressive supportive care. In most
developing countries, gram-negative bacteria remain the major
source of infection and gram positive microorganisms have been
implicated in developed countries, as the most common cause of
neonatal sepsis .While culture positive neonatal sepsis in the USA
is 0.98% but in very low birth weight infants under prolonged
intensive care the culture proven sepsis may beashigh as 30%
[3]. Neonatal sepsis is one of the commonest cause of perinatal
mortality in the developing world. Mortality rate of early onset
neonatal sepsis is 2 to 40% and late onset neonatal sepsis is 2 to
20% .Definitive diagnosis of neonatal sepsis is based on positive
blood or cerebrospinal fluid (CSF) cultures, both of which take at
least 24 to 48 hours and are often falsely negative. Due to irrational
use of antibiotic, sensitivity pattern of microbes are also changed.
In many situations, conventional antibiotics are not sensitive to
causative micro-organisms & developed increased drug resistance
making treatment extremely difficult. Thus, local epidemiology of
neonatal sepsis should be constantly updated to detect changes
in the pattern of infective pathogens and their susceptibility to
various antibiotics. Objectives of the study were to identify the
causative organisms causing neonatal septicemia and to detect
culture-sensitivity of the microorganisms.
Methodology
This is a hospital based prospective case series study which
was performed in Neonatal intensive care unit (NICU), Chittagong
Medical College Hospital, Bangladesh. Duration of this study was
January 2013 to July 2014.and sample size was300. Inclusion
Criteria were Term and preterm babies irrespective of sex and
weight, clinically diagnosed neonatal septicemia patient under
antibiotic treatment and also without, prior antibiotic therapy
included in this study. Exclusion Criteria were severe perinatal
asphyxia, neonate with congenital anomalies, extremely low birth
weight neonates and respiratory distress syndrome.
A baby with good primitive reflex, activity and breast fed in
initial 48 hours of life, who then became sick were considered
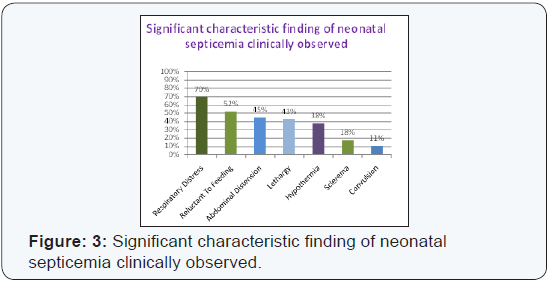
as neonatal sepsis. Characteristic findings of neonatal sepsis
patients were respiratory distress in the form of tachypnoea
and or severe chest in drawing, reluctant to feeding, abdominal
distension, lethargy, hypothermia, Sclerema, Convulsion. On the
day of admission, from every case 3 ml of blood was collected
from peripheral vein with asceptic condition and introduced
into aerobic and anaerobic media. The blood culture specimens
were sent and processed according lyin Bact/ Alert 3D system in
Microbiology laboratory. Departmental ethical committee gave
consent to carry on this study and consent also taken from parents
of this study cases.
MResult
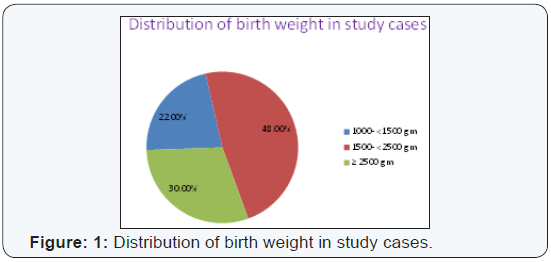
All the cases were grouped into three : Normal birth
weight babies (NBW) (wt ≥2500g) was 30%, Low birth weight, LBW(1500-2500g) was 48% main bulk of patient in the study
cases and very low birth weight babies, VLBW(1500-1000g) was
22% (Figure: 1). In NBW group 57.8% were male and 42.2% were
female. In LBW group 53% were male whereas 47% were female.
In VLBW group 52.8% were male with 47.2% were female. Male
female distribution was statistically insignificant. In NBW group
early onset sepsis (EONS) was 42.2% but in late onset sepsis
(LONS) was 57.8%. In LBW group EONS was 68.2% but late onset
Sepsis 31.8%.
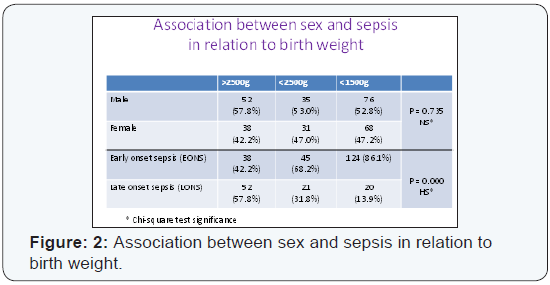
In VLBW group, EONS was 86.1% but in LONS was 13.9
(Figure 2). Characteristic clinical findings of neonatal sepsis
patients were respiratory distress 70%, reluctant to feeding
(52%), Abdominal distension (45%),lethargy (43%),hypothermia
(38%), Sclerema (18%),Convulsion (11% (Figure 3) Early
onset sepsis was more common in study population which was
statistically significant. Serial C-reactive protean is a highly
sensitive marker for neonatal sepsis. In this study 78%.of sepsis
cases were positive for C-reactive protein but 100% of culture
positive cases were positive for C-reactive protein. In this study,
32% cases were culture positive but 68% cases were culture
negative which were clinically sepsis, out of 300 cases, culture
positive only 96 (32%), where Klebsiella (54.17%), Pseudomonas
Aeruginosa (16.67%), Acinetobactor (14.58%), staphylococcus aureus (6.25%), Escherichia coli (6.25%) with mixed infection
Escherichia coli with coliform (2.08%) (Figure 4). Culture
sensitivity of Klebsiella to ciprofloxacin (78%) Imipenem (65%)
Levofloxacin (50%), Meropenem (45%), Cefotaxime(40%),
Ceftazidim (38%) (Figure 5). Sensitivity of pseudomonas to
(69%), Ceftazadim (50%) and Ciprofloxacin (45%) (Figure 6). It
was also observed that sensitivity of Acinetobactor to Amikacin
(81%) Ciprofloxacin (65%), Imipenem (58%), Meropenem
(55%) and Netilmycin (60%) (Figure 7) respectively. Culture
sensitivity of staphylococcus aureus to Vancomycin (83%),
followed by Amikacin 60%, Meropenem (60%), Imipenem (55%)
and Gentamicin (48%) (Figure 8). Culture sensitivity of E. coli
to Amikacin (87%), Ciprofloxacin (75%) and Ceftazidim (55%)
(Figure 9).
Discussion
The cases were grouped into three:- Normal birth weight
(NBW) were 30%, 48% were low birth weight (LBW) and 22%
were very low birth weight (VLBW) babies. LBW (70%) babies
were vulnerable to neonatal sepsis which is similar to other
studies. Early onset neonatal sepsis (EONS) was more common
than late onset which is consistent with other studies. In this
study 78% cases were positive for C-reactive protein but 100%
were positive in culture positive cases. Study of west B. A [4] in
port Hurcourt Nigeria observed that Klebsiella pneumonia (50%),
staphylococcus aureus (21%) were predominant microbes and
sensitive to Ciprofloxacin 88.8%, 99.8% respectively but in our
study Klebsiella pneumonia (54.17%), pseudomonas aeruginosa
(16.67%) were predominant microbes and staphylococcus
aureus (6.25%) but Klebsiella was mostly sensitive to
ciprofloxacin (78%). In the study of Mehroety et al. [5] in Turki
found that staphylococcus aureus (44 %), Klebsiella (10.5%)
were predominant microbes and sensitive to vancomycine and
carbapenem, ciprofloxacin respectively. They noticed fungal
infection was 19.2% in their study. Sensitivity pattern is also
similar to our study but pattern of organisms varies. Shah and Desai
[6] observed in their study E. coli with Klebsiella pneumonia were
predominant organisms caused neonatal sepsis but in our study
Klebsiella with pseudomonas were the predominant organisms and most of the gram negative organisms were sensitive to
Amikacin, Imipenem and gram Combined drugs piperacillin and
tazobactum, which were consistent to our study but we observed
along with above drugs ciprofloxacin and Levofloxacin were also
sensitive. Ramesh & Lincy [7] found in their study 28.8%cases
were blood culture positive and common isolated organisms were
Klebsiella followed by pseudomonas and higher resistance to the
commonly used 1st line antibiotics Ampicillin and gentamicin.
Our study almost consistent to this study. Samia, et
al. [8] where
identified negative organism were the most common pathogens,
80%, were Klebsiella pseudomonas (35%) Enterobator (2%) and
gram positive organisms were staphylococcus 10% and GBS 10%.
But in our study, GBS not detected in any blood culture growth.
In the study of Viwanathan, et al. [9] found in their study gramnegative
organisms were the main causes of neonatal sepsis and
those organisms were almost 100%resistent to conventional
Ampicillin and Gentamicin. Their study findings were similar
to our study. In the study of Sharifun & Afroza, et al. [10] at
Dhaka, Bangladesh observe Pseudomonas, E-coli and coagulase
negative staph common pathogens of neonatal sepsis but in
our study pseudomonas, Klebsiella, AcinetobactorE-coli were
common pathogens but Anti biotic sensitivity almost similar. In
the study of Sharma & Agarwal [11] isolated organisms were
staphauras, Klesiella, E-Coli and their study also mimic to this
study. Staphylococcus auras Agarwel & Bhat [12]. Observed that
32.72% were blood culture positive and common bacteria isolated
were Klebsiella, E-coli and Staphylococcus aureus. No single group
B-streptococcus. (GBS) growth found in blood culture.Limitation
of this study was small size sample from one NICU & Blood culture
done from a number of cases after antibiotic therapy. There was
no conflict of interest. We acknowledge Principal, Director of this
institute and neonates who gave opportunity to carry out this
study.
Conclusion
Microorganisms identified causing neonatal septicemia in
our region are Klebsiella, Acinetobactor, E. coli and Enterobector.
Antibiotics sensitive to identified micro organism were Amikacin,
Ciprofloxacin, Levofloxacin, Imipenem, Meropenem, Vancomycin,
Ceftazidim. Conventional Ampicillin sensitivity is not detected and
Gentamicin sensitivity is also low. Multi centre broad based study
for blood culture sensitivity is essential to guide antibiotic regime
for neonatal septicemia in developing and developed countries.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment