Meropenem Induced Anaphylactic Shock in a Newborn and Review Of Literature Meropenem-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
All drugs have the potential cause to side effects
and anaphylaxis.The bioavailability of the drugs is different in
newborns. Therefore has the tolerability and efficacy of the
medicationsin the newborn period more importance. Meropenem is a
broad-spectrum antibiotic used to treat a wide variety of infections. We
describe here a neonate who developed anaphylactic shock after use of
intravenous meropenem.This is the first reported case of a neonate which
develop anaphylactic shock after meropenem administration.
Objectives: To establish normative data for fine motor developmental skills that can be applicable to Egyptian children.
Conclusion: Clinicians should be
aware of the potentially fatal adverse effects by use of meropenem in
newborns. The rapid intervention of anaphylactic shock saves lives in
all age groups.
Keywords: Anaphylactic shock; Meropenem; NewbornAbbreviations: CRP: C-Reactive Protein; IgE: Immunglobulin E; Min: Minute; NICU: Neonatal Intensive Care Unite; PMNs: Poly Morpho Nuclear leukocytes; TEN: Toxic Epidermal Necrolysis
Introduction
Anaphylaxis is a serious, potentially fatal, systemic
allergic reaction that occurs suddenly after contact with an allergic
substance and may cause death. The rate of anaphylaxis is increasing
yearly, particularly during the first years of life. Newborn infants are
less likely to develop anaphylaxis because of their insufficient immune
response. Common triggers are foods, medications, and insect stings.
All drugs have the potential cause to side effects and anaphylaxis. The
global rate of anaphylaxis in the general population is unknown. The
prevalence based on international studies varies between 0.05-2% [1].
There is an evidence that these reactions are increasing. Serious
adverse drug reactions rose 2.6-fold in the last decades, up to 15% of
them have their hospital stay prolonged. About 10% of the general
population claim to have a penicillin allergy. It’s difficult to
determine the true prevalence, an estimated frequency of penicillin
anaphylaxis is reported by 1-5 per 10.000 cases [2].
Penicillin belongs to an important group of
antibiotics called beta (ß)-lactam antibiotics. This class of
antibiotics includes penicillin and penicillin derivatives such as
ampicillin and amoxicillin as well as cephalosporins, monobactams,
carbapenems and ß-lactamase inhibitors. Penicillin derivatives can also
cause to allergic reactions such as penicillins [3,4]. Newborns are less
likely to develop anaphylaxis because of their weak immunoglobulin E
(IgE)-mediated immunity and nonimmune mechanisms [2,5]. The true
incidence of immunoglobulin (Ig)E-mediated cross-reactivity is not known
exactly. Cross-reactivity reactions between penicillins and carbapenems
for IgE-mediated are very rare reported [6]. We described here the
first case of a newborn who developed anaphylactic shock after
administration of intravenous meropenem.
CASE REPORT
A female newborn baby weighing 2690g (10-25th
percentile) was born to a 21 years old mother by caesarean section at
36+2 weeks gestation. After birth, she was hospitalized with a diagnosis
of polycythemia and transient tachypnea at our neonatal intensive care
unit (NICU). Physical examination on admission revealed tachypnea with a
heart rate of 158beats/min and respiratory
rate of 72/min. The rest of systemic examination, blood pressure
measurements and oxygen saturations were in normal range. The
baby was kept under warmer with an oxygen replacement of 4L/
min. Arterial blood gas examinations are in normal range. She had
a high hematocrit level (69%) at admission, and was treated with
intravenous fluid therapy. Blood count and CRP values were also
in the normal range.
After four day follow uprising in CRP (5.1mg/dL) values are
detected. Meropenem treatment was started after septic work up,
but the newborn developed 10 seconds after 20mg/kg intravenous
administration of meropenem (Meropenem 500mg/5mL;
AstraZeneca Ltd. Şti., Istanbul, Turkey) erythematous rashes and
urticaria. The rashes began from the scalp and invaded the entire
body in about few minutes (Figure 1). The newborn developed
tachypnea, tachycardia and angioedema.Moderate metabolic
acidosis (pH: 7.29, pCO2: 52mmHg, pO2: 35mmHg, HCO3:
14mmol/L, base excess: -6mmol/L) and respiratuvar distress was
also presented. The blood pressure measurements are hypotensive
(before and after meropenem administration the blood pressure
was 75/45mmHg, mean 51mmHg; after 29/12mmHg, mean blood
pressure 20mmHg, respectively). Prothrombin and activated
partial thromboplastin times were within normal range.High-flow
oxygen (through mask) was used for respiratory symptoms and
hypoxemia at crisis.

The patient was treated with 10cc/kg NaCl 0.9% bolus
intravenous fluid infusion in 20 minutes, intramuscularly
epinephrine with a dosage of 0.01mg/kg (0.1mL/kg of 1:10.000)
and 1mg/kg methylprednisolone. His blood pressure values
increased after treatment spontaneously. The rashes began to fade
in the first hours, and his blood gases normalized after 60minutes
(Figure 2). Investigations showed normal urea, electrolytes,
glucose, calcium, magnesium, and liver function tests. The blood
tests show a leucocyte count of 8.56x109/L with 56% PMNs and
30% lymphocytes and %8 eosinophilia. Penicillin specific IgE
values are elevated (3.5kU/I) and high serum tryptase level 22ng/
mL (2-11.5ng/mL) was observed. Skin tests couldn’t performed at the
patient. There was no history of allergy in the medical history.
Bloodcultureswere sterile. The patient was discharged after a
prolonged hospitalization at the second week of life. The parents
are advised to avoid the use of meropenem for any indications and
follow-up at child allergy specialist was recommended.

Discussion
We describe here the first case of a newborn who developed
anaphylactic shock after intravenous meropenem administration.
Meropenem is a broad-spectrum antibiotic used to treat a wide
variety of infections. It’s a β-lactam group antibiotic and belongs
to the subgroup of carbapenems. The spectrum of meropenem
includes many of Gram-positive, Gram-negative and anaerobic
bacteria. The mostly observed side effects of this drug are
constipation, diarrhea, vomiting, rashes, headache, inflammation
at injection site; rarer side effects are apnea, angioedema,
erythema multiforme, leukopenia, pleural effusion, Stevens
Johnson syndrome, and toxic epidermal necrolysis (TEN) [7].
Meropenem anaphylaxis in newborn is previously not reported.
Anaphylactic reactions are rare in newborns because of their weak
immunoglobulin E (IgE)-mediated immunity and nonimmune
mechanisms [1-3].
The presentation signs of anaphylaxis in newborns are usually
sudden infant death syndrome, poor sensorium, flaccidity, apnea
and cyanosis. The majority of anaphylactic reactions involves
skin reactions. Other affected organ systems are respiratory,
gastrointestinal, cardiovascular and central nervous system.
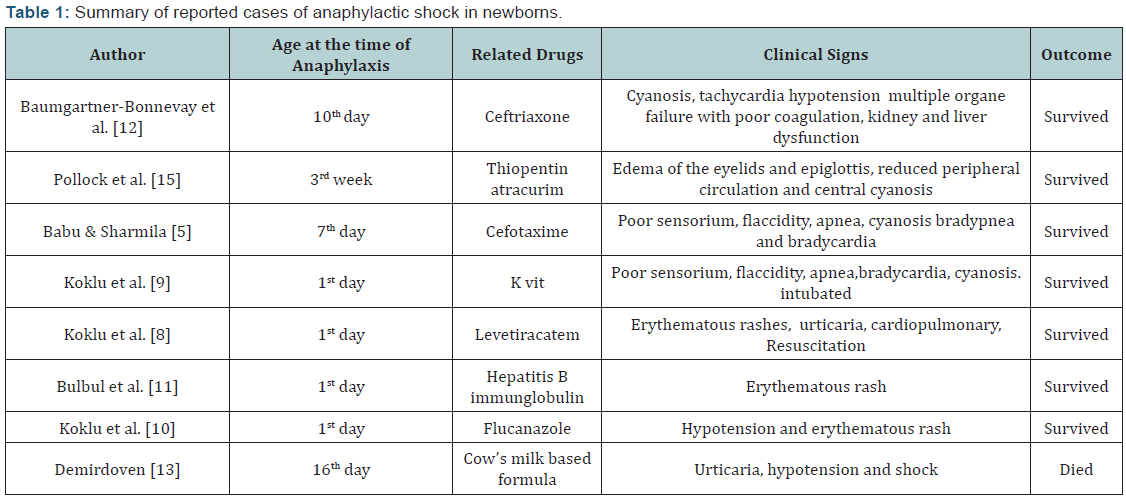
Koklu et al. [8-10] reported three cases of anaphylaxis in the
first days of life due to levatiracetam, K vit and flucanazole. Rare
cases of anaphylaxis or anaphylactic shock in newborns caused to
hepatitis B immunoglobulin, cefotaxime, ceftriaxone, thiopentone,
atracurium, flucanazole, K vit and levatiracetam have been also
reported. Recently was an anaphylactic shock due to a cow’s milkbased
formula in a newborn reported, but all these cases show
timely intervention avoid the death in any of these anaphylactic
reactions (Table 1) [11-13].
Anaphylaxis is a life-threatening reaction which developed
over few seconds-minutes to hours with multisystem involvement.
It’s usually triggered by an agent such as food, insect sting, latex
or medication, through a mechanism involving immunoglobulin
E (IgE), mast cells eosinophils and basophils [1,3]. The diagnosis
of anaphylaxis in newborn is difficult because their immune
system is immature. Anaphylaxis is a primarily clinical diagnosis,
laboratory tests are rarely helpful. There are no tests available in
an emergency department to confirm a diagnosis of anaphylaxis
in the real time. The diagnosis of anaphylaxis during the acute
event is based on clinical presentation and history of a recent
exposure to an agent. The tests to find what substance or allergen
may trigger the allergic response are usually skin or blood tests.
Laboratory tests in serum, plasma, and urine are also helpful in
the further diagnosis.
The principal effector cells of systemic anaphylaxis are mast
cells and basophils [4,6]. Mediators like tryptase and histamine
are released by mast cells and basophils during anaphylaxis.
Tryptase is the most abundant secretory granule-derived serine
proteinase contained in mast cells and can be used as a marker for
mast cell activation. Elevated serum tryptase values are detected
in anaphylactic and anaphylactoid reactions, but the negativity
cannot exclude the anaphylaxis [1,14]. Blood tests are not sensitive
than skin tests, but could be used in patients who are not able to
have skin tests. The most common type of blood tests are enzymelinked
immunosorbent assay (ELISA, EIA), radioallergosorbent
testing (RAST) or immunoassay capture test and blood level of
a type of antibody (called immunoglobulin E, or IgE) can help to
confirm the diagnose of anaphylaxis. Blood tests revealed elevated
tryptase levels in our case too. Anaphylaxis is a clinical emergency,
and all healthcare professionals should be able with its recognition
and acute and ongoing management. Rapidly intervention has
importance in save of lives. Successful management of anaphylaxis is based on early diagnosis and treatment. Epinephrine given
intramuscularly remains the mainstay of treatment for this
condition. Other second-line therapies, such as inhaled beta-2
agonists, H1 and H2 receptor antagonists and corticosteroids,
may play a role in resolving respiratory and cutaneous signs and
symptoms [2,4,6]. The symptoms in our patient resolves quickly
by administration of epinephrine, antihistamines and steroids.
Long-term risk reduction in patients with anaphylaxis focuses
on optimal management of relevant comorbidities and relevant
immunomodulation [3,14]. We could not found any reports of
neonatal anaphylactic shock due to intravenous administration of
meropenem in the literature. Our presented case takes attention
to anaphylactic shock by use of meropenem in newborns.
Conclusion
Anaphylaxis is a clinical emergency and could be seen in
different groups. All healthcare professionals should be able with
its recognition and acute and ongoing management. Meropenem is
a commonly used broad spectrum antibiotic which could develop
fatal anaphylactic reactions in newborns. Clinicians should be
aware of the potentially fatal adverse effect by use of intravenous
meropenem. The rapid intervention of anaphylactic reactions
saves lives in all age groups.
Compliance with Ethical Standards
Funding: This case has been written without support of any
found.
Disclosure of Potential Conflicts of Interest
The authors declare they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants
included in the case.
Acknowledgement
Hakyemez Toptan H, Karadag N: Writing (all sections), case
and review design, editing (introduction, what’s known, what’s
new, discussion), revising writing (all sections), Akar S: writing,
editing. Dogru M: Child Allergy Specialist, GokmenYildirim T:
Writing (all sections), case and review design, editing, Dogru M:
Pediatric allergy counseling, Ozalkaya E, Karatekin G: Case design,
editing.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment