Pulmonary Hypertension in Children with Esophageal Varices: Frequency and Relation to N-Terminal Pro B-Type Naturetic Peptide-Juniper publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Background:Portopulmonary
hypertension (PPHTN) is a distinct pulmonary vascular complication of
portal hypertension. There is no much information on PPHTN occurring in
children. Detection of PPHTN at an early stage requires systematic
screening at regular intervals by echocardiography (ECHO) in children
with portal hypertension.
Aim of the work:to study the
frequency of PPHTN in children attending Assiut University Children
Hospital with esophageal and/ or fundal varices, to measure serum levels
of Human N-Terminal Pro B-type Naturetic Peptide (NT-proBNP) and to
evaluate its correlation with the occurrence of pulmonary hypertension
in these children.
Patients and methods:This cross
sectional study included 40 children with portal hypertension and 20
controls. All children with portal hypertension underwent Pulse oximetry
and echocardiographic studies (ECHO). Serum levels NT-proBNP was
measured in all cases and controls.
Results:6 (15%) were diagnosed as
PPHTN. Dyspnea on exertion was detected in four children with PPHTN
(66.7%), hypoxia was not detected in any of them. NT-proBNP was not
significantly higher in children with portal hypertension than controls.
There was no significant correlation between peak systolic pulmonary
artery pressure (SPAP) and ALT, nor NT-proBNP. Circulating Levels of
NT-proBNP did not correlate significantly with a right ventricular
diameter or right ventricular anterior wall diameter.
Conclusion:Portal hypertension is an
important risk factor of development of pulmonary hypertension in
children. ECHO is a non invasive, safe and reliable screening method for
children with PPHTN. Further researches are needed to evaluate the
diagnostic and prognostic values of NT-proBNP in these children.
Keywords:Pulmonary hypertension; Children; Esophageal varicesIntroduction
TThe vascular set of the liver is unique. The portal
vein reaches the liver, where it branches into the liver sinusoids and
comes out of the liver as hepatic veins which pours the blood into the
inferior vena cava hence to the right atrium and right ventricle. From
the right ventricle arises the pulmonary artery that carries the blood
to the lungs. It can be therefore understood that rises in portal vein
pressure, especially with the occurrence of portosystemic varices would
lead to a secondary rise in the pulmonary arterial pressure. So that
Portopulmonary hypertension (PPHTN) is a distinct pulmonary vascular
complication of hepatic and extrahepatic portal hypertension in the
absence of underlying cardiopulmonary disease [1-6]. The end result is a
progressive remodelling of the wall of the small pulmonary arteries
with vasoconstriction and thickening of the arterial wall resulting in a
histopathological pattern of plexogenic arteriopathy. Because clinical
symptoms are nonspecific and often subtle, a high index of suspicion for
diagnosis is required [7]. PPHTN has chiefly been studied in adults
[3]. There is not much information on PPHTN occurring in children; it
has been reported in children with portal hypertension resulting from
both cirrhosis and from congenital or acquired portal vein
abnormalities. However, most reports deal with a small number of
patients, and little is known of its prevalence and severity in children
with liver disease [7,8]. Detection of PPHTN at an early stage requires
systematic screening at regular intervals by echocardiography (ECHO) in
children with portal hypertension. A careful ECHO surveillance of
pulmonary artery pressure must be set up in such patients to allow early
diagnosis and treatment of PPHTN. ECHO is the most widely used
screening method for the detection of pulmonary artery hypertension
(PAH). It provides a reasonably reliable and comprehensive assessment of
the right
heart and the pulmonary circulation [9].
Human N-Terminal Pro B- type Naturetic Peptide (NT-proBNP)
is released from the ventricles in response to volume and pressure
overload and serves as a noninvasive marker of right ventricular
systolic impairment [10]. Recent attention has focused on these
biomarkers as a potential screening tool for early pulmonary
artery hypertension (PAH) in high-risk populations [11].
Aim of the Work
To study the frequency of PPHTN in children attending Assiut
university children’s hospital with esophageal and/ or fundal
varices due to portal hypertension, to measure serum level of
NT-proBNP and to evaluate its correlation with occurrence of
pulmonary hypertension in these children.
Patients and Methods
This cross sectional study included 40 children with portal
hypertension (24 males, 16 females) and 20 apparently healthy
age and sex-matched children as a control group. Patients were
consecutively recruited from pediatric gastrointestinal endoscopy
unit of Assiut university children hospital during the period from
January 2013 to December 2015. The only inclusion criterion was
the presence of portal hypertension diagnosed by endoscopic
evidence of esophageal and/or gastric varices. All patients with
histological evidence of cirrhosis, or Doppler ultrasonography
evidence of portal vein thrombosis or cavernous transformation
of the portal vein were included in this study. Patients were
excluded if they had primary lung or heart disease, Budd-Chiari
syndrome or spleen resection. This study was approved by the
Ethical Committee of the Faculty of Medicine, Assiut University,
according to the latest revision of the Declaration of Helsinki, and
informed consent was obtained from participants’ parents/legal
guardians. All studied children were subjected to full history taking
through clinical examination, including age, gender, duration of
illness, underlying diagnoses, causes of portal hypertension, prior
complications and management of portal hypertension. Physical
examinations were performed to evaluate for clinical evidence of
portal hypertension and any clinical evidence of PAH.
Complete blood count measured using the CE11–DYN 3700
spectra–USA apparatus, liver function tests measured using a
Synchron CX Pro auto-analyzer, Beckman Counter (Tokyo, Japan),
prothrombin time and concentration and international normalized
ratio (INR) were obtained. 3ml of venous blood samples were
collected from patients and controls under standardized
conditions in plain tubes were centrifuged (at 3000 g for 10min.)
and serum samples were divided and stored in aliquots at – 20
°C until analyzed. Assay of serum levels of Human N-Terminal
Pro B-type Naturetic Peptide (NT-proBNP) was performed using
ELISA Kit (from WKEA Med Supplies-China catalog.No.WH-
219Lot No.20151119).
Pulse oximetry was used to screen for hypoxia in all
patients.
Arterial oxygen saturation (the amount of oxygenated hemoglobin in the
blood) was recorded using a portable, battery powered pulse
oximeter (Mini SPO2T manufactured by the Medair Hudiksvall,
Sweden; Ref. LS1P- 9 Q) with the sensor device placed over the
finger (index or middle) or the big toe. A reading that was stable
for at least 3 minutes was noted down. Hypoxemia was defined as
an arterial oxygen saturation of 90% recorded by pulse oximetry
[12].
Evaluation for PPHTN
All children with portal hypertension underwent
echocardiographic studies using M– mode, two dimensional, and
Doppler techniques using commercially available phased array
system employing a 4 and 7 MHZ transducer respectively (Magic
bright 2, Vivid 3, Vingmed-Tech). Measurements were performed
using the machine’s incorporate analysis package. Standard
echo assessment was done using the standard parasternal view
(longitudinal and transverse), apical view 4 and 5 chambers, also
subcostal and suprasternal views.
On the echocardiography scan, special attention was given to- Right ventricular Size This was measured in the m-mode parasternal short axis biventricular view [13].
- Interventricular septum. If there was a D shape in RV in parasternal short axis view [14].
- Hemodynamic assessment using Doppler echocardiography.
- Systolic pulmonary artery pressure (SPAP). Tricuspid regurge jet exceeding 2.5m/Sec considered significant. Systolic pulmonary artery pressure estimated from a peak tricuspid regurg velocity by a continuous wave Doppler using the modified Bernoulli equation to determine the RV systolic pressure. RVSP=SPAP=4(TRmax)2 + mean RA pressure (m RAP). A proper angulation and a sufficient envelope were taken in apical views [15].
- Diastolic pulmonary artery pressure. The diastolic pulmonary artery pressure (DPAP) was estimated from the velocity of the end-diastolic pulmonary regurgitant velocity using the modified Bernoulli equation: DPAP=4V (enddiastolic pulmonary regurgitation velocity square)2 + RA pressure [14].
- Mean pulmonary artery pressure. mPAP=4V (Early peak pulmonary regurgitation velocity)2 + RA pressure. This equation has been shown to correlate well with invasive measurements in adults and children [16].
The normal estimated systolic pulmonary artery pressure
(SPAP) is >35mmHg [17]. Mild PAH can be defined as an SPAP of
approximately 36–50mmHg [18].
Statistical Analysis
Categorical variables were described by number and percent
(N, %), while continuous variables were described by mean and
standard deviation (Mean, SD and Median).
The chi-square test was used to compare categorical variables.
Continuous variables were tested for normal distribution, using
Kolmogrove Smirnov test and Q-Q Plots. To compare between
continuous variables t-test (parametric test) and Mann Whitney
U test (non-parametric test) were used. Kruskal-Wallis H used for multiple comparisons. Pearson Correlation coefficient used to
assess the association between continuous variables.
A two-tailed p0.05 was considered statistically significant.
All analyses were performed with the SPSS 20.0 software.
Results
Kruskal-Wallis H (nonparametric test) used to compare between all
studied groups, Mann Whitney U (non parametric test) used to compare
between each two groups).
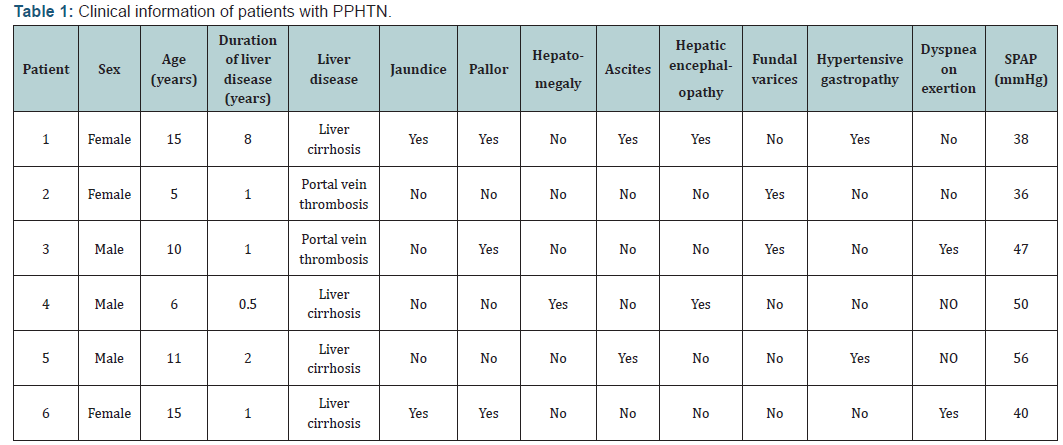
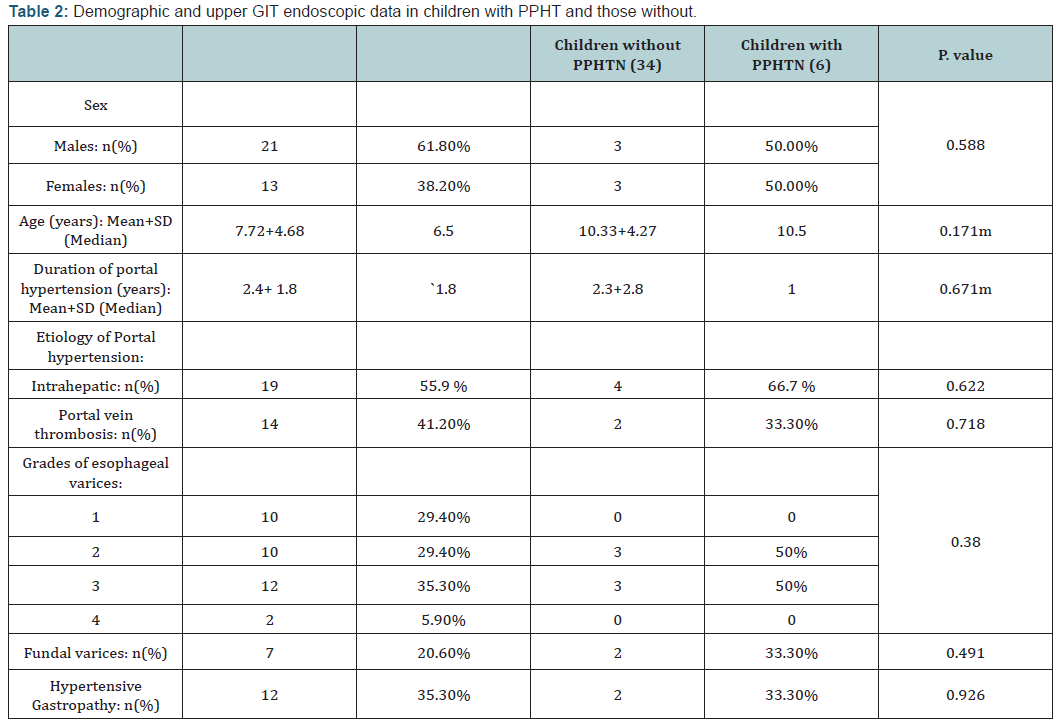
Among 40 children with portal hypertension included in this
study, 6 (15%) were diagnosed as PPHTN (SPAP >35mmHg). Our
results are shown in Tables 1-4. Regarding the clinical signs of
pulmonary hypertension, dyspnea on exertion was detected in four
children with PPHTN (66.7%), other clinical signs of PAH were not
detected in any of them. Using pulse oximetry, hypoxia (arterial
oxygen saturation of 90%) was not detected in any of children
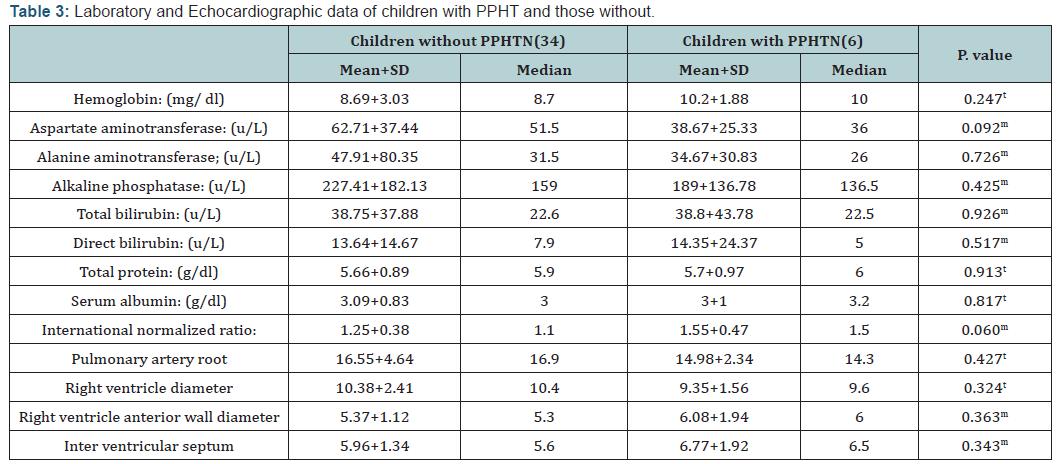
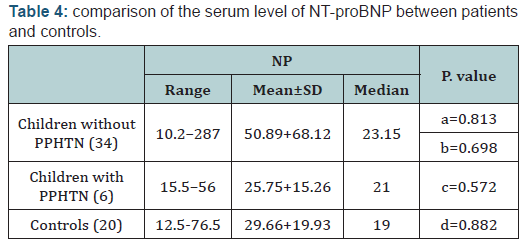
with PPHTN. The results of this study demonstrated that there is
no statistically significant difference in serum levels of NT-proBNP
between children with PPHTN and those without. In addition,
circulating Levels of NT-proBNP did not correlate significantly
with PSAP, right ventricular diameter or right ventricular anterior
wall diameter (r=0.154; p=364), (r=0.192; p=0.236) and (r=0.093;
p=0.567) respectively. Furthermore, there was no significant
correlation between SPAP and ALT (r=0.1; p=0, 54)
Discussion
PPHNT is an important consequence of portosystemic
shunting in children with chronic liver diseases or with extra hepatic
portal vein obstruction/thrombosis. It is essential to be
recognized early to prevent irreversible vascular remodelling [19]. Only
small series of affected children have been reported and the
incidence and clinical features of PPHTN in children have not been
adequately described [20]. Out of 40 children included in this study,
we report a series of 6 (15%) children with PPHTN. Our figure is
higher than that reported by previous authors [7,8,19,21,22]. This
difference may be due to the difference in the inclusion criteria
between different studies or the difference in methods of PPHTN
detection. In the present study, we included children with portal
hypertension complicated with hematemesis due to esophageal
and /or fundal varices, which may explain the high percentage of
children with PPHTN in this study. Regarding screening of PPHTN,
currently there is no accepted universal screening protocol
for PPHTN in children with portal hypertension [7]. Although
diagnosis of pulmonary hypertension is traditionally obtained by
right heart catheterization (RHC) [23,24]; which is an invasive,
risky procedure in small children and bleeding complications are a
concern among patients with liver disease, other forms of diagnosis
are preferred [20]. In the present study the children were screened
by ECHO because it is non invasive, safe, reliable and previous
studies reported that results of ECHO are comparable to RHC in
patients with pulmonary hypertension [25,16]. Furthermore
the European Respiratory Task Force’s recommended ECHO as a
screening test for PPHTN [26]. The present study shows that there
was no statistically significant difference between children with
PPHTN and those without regarding demographic or laboratory
data. These results are different from previous studies who
reported that females [27] and low hemoglobin level [20] are
risk factors, but agree with other study [28] who stated that the
presence of portal hypertension and portosystemic shunts are
thought to be the single most important factors determining the
risk of development of pulmonary hypertension. Regarding the clinical
pictures and severity of PPHTN in children included in this
study, fortunately most cases (83.3%) with PPHTN diagnosed in
this study were mild (PSAP 50mmHg). Furthermore, the clinical
signs of pulmonary hypertension were not detected in our patients
except dyspnea on exertion in four children with PPHTN (66.7%)
which is a nonspecific symptom. Hypoxia was not detected in
any of them. In the present study, we screened for hypoxia using
pulse oximetry because of its non-invasive nature in order to
avoid obtaining arterial blood gas measurements because of
ethical consideration and previous studies reported that SaO2 by
pulse oximetry is an appropriate alternative to arterial blood gas
measurements to screen children with portal hypertension [21].
In the present study only one child (16.7%) had SPAP 56mmHg;
interestingly he did not have any clinical sign of PAH. Because our
policy is avoiding invasive procedure in these children unless they
will achieve a great benefit and this child is already suffering from
chronic liver affection, we avoided the idea of doing RHC to this
child.
The results of the present study showed that there was no
significant correlation between PSPA with liver function. These
results are in agreement with previous study [20] however, these
results are based on small number of cases and large studies are
required to verify this correlation.
NT-proBNP are cardiac biomarkers released by myocytes
in response to ventricular wall stress due to pressure overload
and volume expansion [29,30]. The value of these biomarkers in
the diagnostic approach of PAH has already been investigated in
adults, with promising results. In some studies, there is increasing
evidence that NT-proBNP may be a useful marker for right
ventricular dysfunction and predict outcome in patients with PAH
[31,32]. Circulating levels of NT-proBNP correlate with mPAP [33].
While in others there is not enough evidence to rely on BNP as
a diagnostic marker of patients with PAH [34]. Pediatric studies
are still scarce [27]. The results of this study demonstrated that
NT-proBNP was not significantly higher in children with PPHTN
than those without. Furthermore, circulating Levels of NT-proBNP
did not correlate significantly with PSPA. Casserly et al. [32]
reported that elevations in NT-proBNP levels are usually not seen
until pulmonary artery pressure is high enough to cause right
ventricular strain. In this study, all cases with PPHTN diagnosed
were mild and this may explain the absence of significant
elevation of circulating levels of NT-proBNP in children with
PPHTN than those without. The usefulness of these biomarkers
in clinical care is also still a debate, some authors stated that
these biomarkers do not replace the clinical parameters, but may
provide additional information [35]. Others reported that both
baseline levels of plasma BNP and its increase during a 3-month
follow-up period are strong independent prognostic factors in
patients with PAH [36]. So, further research would be needed to
assess the diagnostic and prognostic values of the biomarkers.
Finally, important issues regarding screening and management of
PPHTN in children remain unanswered. There are no controlled,
prospective studies that have addressed the question of which medications are most efficacious and safe in PPHTN patients.
Whether liver transplantation should be used for treating a child
with PPHTN complicating or whether PPHTN should be treated by
pulmonary vasodilators remains open to discussion [8,37].
Conclusion
Portal hypertension is an important risk factor of development
of pulmonary hypertension in children. ECHO is a non invasive,
safe and reliable screening method for children with PPHTN.
Further researches are needed to evaluate the diagnostic and
prognostic values of NT-proBNP in these children.
Funding
Available resources of Assiut University.
Conflict of Interest
No conflict of interests.- All authors declare that the submitted version of this paper is original and is not under simultaneous consideration for publication elsewhere and tables in this study did not reproduced from another source.
- All authors have seen and agreed to the submitted version of the paper in this journal
- All Authors declare that there are no conflicts of interest and source of funding is the available resources of Assiut University.
- This study was approved by the Ethical Committee of Faculty of Medicine, Assuit University according to the latest revision of the Declaration of Helsinki and informed consent was obtained from participant’s parent/legal guardian.
Author’s Contributions
DR Nagla Abu Faddan who collect the scientific data for this
study and write the manuscript, Dr Duaa Rafaat, who perform the
Echo examination for all children. Dr Tahra and Dr Madleen who
perform the laboratory work in this study.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment