Acute Steroid Induced Myopathy after Single IM Dose of Steroid-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Introduction:AMS after a single IM
dose of dexamethasone is very rare. And till now no one has reported
similar case, on the other side the chronic myopathy induced by high IV
corticosteroids is not unusual.
Case presentation:A 3 years old
female had acute myopathy with rhabdomylosis after a single dose of
steroid with rapid improvement after discontinued the medication
Conclusion:In spite of that our case
is rare; the physician should pay attention while using steroids,
especially when clinical situation and laboratory tests are highly
suspicious.
Abbreviations:ALP: Alkaline
Phosphatase; ALT: Alanine Aminotransferase; ASM: Acute Steroid Myopathy;
AST: Aspartate Aminotransferase; CPK: Creatinine Phosphokinase; CRP:
C-Reactive Protein; EMG: Electromyography; ESR: Erythrocyte
Sedimentation Rate; IV: Intravenous
Introduction
Steroid myopathy is usually an insidious disease
process that causes weakness mainly to the proximal muscles of the upper
and lower limbs and to the neck flexors. Cushing originally described
it in 1932, and Muller and Kugelberg first studied it systemically in
1959. An excess of either endogenous or exogenous corticosteroids is
believed to cause the condition. Excess of either endogenous or
exogenous corticosteroids is believed to cause the condition [1,2].
Corticosteroids were introduced into clinical
practice in 1948, and in 1958, Dubois [3] reported the first patient
with myopathy resulting from iatrogenic corticosteroids. Since
corticosteroid therapy’s introduction into clinical practice, both acute
and chronic steroid myopathies have been well recognized.
Chronic steroid myopathy is more common and develops
after prolonged usage of steroids [3,4]. Acute steroid myopathy (ASM) is
less common and develops early in the course of treatment, typically
with high-dose intravenous (IV) steroids [4].
Earlier case reports of ASM usually involved patients
with asthma receiving high-dose IV corticosteroids for status
asthmaticus [5]. Geeta A Khwaja also reported on 2009 a case of Acute
Myopathy Following Short-term Low-dose Oral Steroid Therapy in adult
patient [6].
Acute myopathy developing from intramuscular
corticosteroid has not been often reported. No case was found yet that
described a pediatric patient developing myopathy after a single dose of
intramuscular corticosteroid therapy.
Case presentation
A 3 years old, female known case of bronchial asthma
step 1, was in usual healthy state till 3days back when she had upper
tract infection which induced acute asthmatic exacerbation, this episode
was treated by nebulized albuterol (ventolin) and one dose of IM
dexamethasone (0.5 mg /kg /dose), respiratory symptoms improved but
after 24 hours. The patient had generalized muscle weakness and myalgia
with no skin rash or joint problem, after that her urine became dark.
Her mother sought medical advice in our ER, and she
mentioned 2 similar attacks after steroid injections but without urine
color changing.
- On examination, the patient looked ill with stable vital signs, no skin rash
- On examination, the patient looked ill with stable vital signs, no skin rash
- She was admitted for further investigation, where laboratory tests revealed
- ESR=11 mm/h, high liver and muscle enzymes CK =3200 LDH=404 AST=242 ALT=41 ALP=109
- Other serum biochemistry levels and renal function were normal
- Urine dipstick showed 4+ blood, urine analysis confirmed presence if myoglobin.
- Rhabdomyolysis was suspected and treated by adequate hydration and urine alkalizing.
- The patient clinically improved and urine became clear
- Rheumatologist excluded connective tissue disease, including dermatomyositis.
Depending on acute course and rapid recovery neurologists
diagnosed this case as rhabdomyolysis resulting from acute
steroid myopathy.
After 4 days of admission, she was discharged with follow up
as an outpatient.
EMG was done as outpatient and was normal; unfortunately
the nerve conduction study was not done.
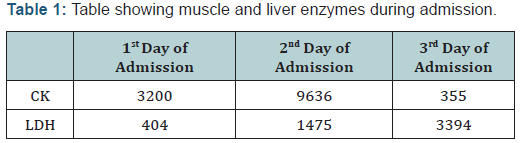
The following Table 1 is showing muscle and liver enzymes
during admission.
After 2 weeks: The patient was doing well with normal
physical examination and LDH =200 CK=250 ALT=44 AST= 53
Discussion
Steroid myopathy may be more frequent with the use of
fluorinated steroids, such as dexamethasone or triamcinolone, than
with nonfluorinated ones, such as prednisone or hydrocortisone.
[5, 6] Although the exact mechanism of the muscle pathology
is unclear, it may be related to decreased protein synthesis,
increased protein degradation, alterations in carbohydrate
metabolism, mitochondrial alterations, electrolyte disturbances,
and/or decreased sarcolemma excitability [1].
Most of studies have shown that myoglobinuria secondary to
drugs, when considered in the pediatrics population, occur more
so in the seconds decade of life, our case elluded to the fact that it
can occur in younger age groups as well [7].
Hypokalemia can induce rhabdomyolysis but in our
patient, hypokalemia, as secondary to perhaps B2 agonist, or
corticosteroids, could not have contributed to the development of
myoglobinuria, as the patient’s biochemistry profile was normal
[8].
The acute form of steroid myopathy is uncommon. It usually
occurs in ICU patients who receive high dose IV corticosteroids
and/or nondepolarising neuromuscular blocking agents to
facilitate mechanical ventilation, but can occur with high-dose
glucocorticoid use alone [6].
Acute, generalized weakness, including weakness of the
respiratory muscles, typically occurs 5-7 days after the onset of
treatment with high-dose corticosteroids.
Generalized muscle weakness, not limited to a more proximal
distribution is noted.
Muscle stretch reflexes typically are normal and sensory
examination should be normal [1]. Though most cases in the
literature report a lengthy prolonged recovery phase sometimes
taking 3-12 months for full recovery, our patient exhibited a rapid
recovery….. one such speed recovery was reported.
In acute steroid myopathy, most patients have high levels
of serum creatine kinase (CK). AST, ALT, as well as associated
myoglobinuria.
Our patient, however fortunately did not develop ARF, as
the serum urea nitrogen and serum creatinine remained within
normal limits. It is recommended that a low threshold of clinical
suspicion be employed; and serum CK as well as urine dipstick
and microscopy to detect myoglobinuria should be obtained for
patients in whom rhabdomyolysis may be possible [9]
in adults is not diagnostically helpful EMG was normal in our case.
Interestingly, gender also seems to be a risk, as women are
twice as likely as men to develop muscle weakness [10]… of
note. Our patient was also a female, hence, there was a gender
predilection for the likelihood of developing drug induced acute
rhabdomyolysis.
Treatment of ASM is aiming to discontinue the rhabdomyolysis
and prevent developing renal failure. No definitive treatment was
found in literature except only to stop giving steroid, in addition to
that weakness seen with steroid myopathy typically resolves after
the corticosteroid dose is reduced or discontinued.
This case revealed clearly that even single IM dose of steroid
can cause ASM.
Conclusion
We think that steroids still a cornerstone of treatment for
most areas of Medicine, and it is unwise to abandon this drug, and
despite the rarity of this case, our clinical threshold should be low
to discover it, even after single dose.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment