Use of an Arterial Cannula in Intubated Children Secondary to Bronchiolitis is Associated with Multiple Blood Gas Sampling and Prolonged Ventilation-Juniper publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Background: Bronchiolitis is a
common cause of respiratory failure in children. Respiratory failure, in
the PICU, is often managed with the utilization of arterial cannulas
and frequent arterial blood gas sampling. Despite the common use of
arterial blood sampling, it is unclear if these tests improve outcomes.
Objective: To evaluate the
frequency of blood draws for blood gas sampling and the duration of
mechanical ventilation in children with respiratory failure with
bronchiolitis in whom arterial cannel as were placed after initiation of
mechanical ventilation.Setting: Children were recruited from a tertiary
care children’s hospital.
Design: Retrospective cohort study.
Setting: TPICU at a tertiary care children’s hospital.
Patients: 109 children between 0 to 2 years with a diagnosis of bronchiolitis requiring mechanical ventilation.
Methods: A retrospective chart
review was conducted on patients ages 0 to 2 years admitted to the PICU
with a diagnosis of bronchiolitis who required invasive mechanical
ventilation between May 2008 and June 2014. Data collected included
demographics, ventilation duration, number and type of blood gases
drawn, PaO2/FiO2 and SpO2/FiO2 ratios at the time of intubation, and arterial cannula related complications.
Results: The mean duration of
mechanical ventilation for patients with an arterial cannula was 7.9
(SEM±0.57) days compared to 5.9 (SEM±0.67) days in patients without an
arterial cannula (p< 0.04). The average number of blood gases drawn
was 2.5 times higher in the arterial cannula group (p< 0.0001).
Conclusion: The presence of
arterial cannulas in children intubated for bronchiolitis is associated
with increased duration of mechanical ventilation and increased
frequency of blood gas sampling.
Keywords: Bronchiolitis; Arterial Cannulas; Arterial Blood Gases; Mechanical Ventilation; Intensive Care Unit
Abbreviations: ABG: Arterial Blood Gas; PICU: Pediatric Intensive Care Unit; MV: Mechanical Ventilation; PaO2: Partial Pressure of oxygen in arterial blood; FiO2: Fraction of inspired oxygen SpO2: Oxygen saturation in blood
Introduction
Arterial cannulas are frequently used for invasive
monitoring in critically ill patients. The most common indications to
place an arterial cannel include the need for frequent blood sampling
and/or continuous blood pressure monitoring. The placement of an
arterial cannula in the management of bronchiolitis is primarily based
on physician preference for blood sampling, as hemodynamic instability
is not common.
Despite advances in non-invasive monitoring,
including automated rapid cycling oscillometric blood pressure devices,
pulse ox meters, transcutaneous oxygen monitoring, and end tidal carbon
dioxide monitors, the utilization of invasive arterial catheters are
still common in PICUs. Annual worldwide usage is reported as up to eight
million in the United States and 2.5 million in Europe [1]. Arterial
blood gases (ABGs) are one of the most common laboratory tests ordered
in the intensive care unit.
Makassar et al demonstrated that the presence of an arterial
catheter was associated with the number of ABGs drawn per
patient independent of all other measures of the patient’s clinical
status [2].
Arterial catheterization, while common in the critical care
setting, is not without significant risks for morbidity. The most
common complications associated with arterial puncture are pain,
arterial injury and thrombosis with distal ischemia, infection,
hemorrhage and aneurysm formation[3]. The incidence of arterial
cannula-related infection in intensive care has been reported as
0.59 per 1000 catheter days with 0.34% developing catheterrelated
blood stream infections [4]. Arterial cannula related blood
stream infections are also associated with serious complications,
including site pseudo aneurysms, septic thromboarteritis and
arterial rupture. These infections carry a considerable risk of
morbidity and mortality, as complications often require surgical
intervention [5].
In addition to complications associated with the use of arterial
cannulas, their use also may increase the financial burden to
providing critical care with questionable added clinical value [6].
Capillary blood gas samples can accurately predict ABG values of
pH, pCO2 and HCO3 for patients with acute respiratory failure
being treated with mechanical ventilation and do not require the
placement of an invasive catheter [7].
Bronchiolitis is a common cause of respiratory failure in
children, often necessitating admission to the pediatric intensive
care unit (PICU) and invasive mechanical ventilation[8].
Respiratory failure secondary to bronchiolitis is often managed
with the assistance of arterial cannulas and frequent ABG
sampling. Despite the common use of ABGs, it is unclear if frequent
blood gas sampling improves outcomes. In our institution we have
observed that there is a disparity in clinical practice among PICU
attending physicians with regards to the use of arterial cannulas
and ABGs to determine clinical care and the pace of weaning
patients off mechanical ventiliation in children intubated for
respiratory failure secondary to bronchiolitis. In this retrospective
cohort study at a single center tertiary care PICU, we evaluate the
relative frequency of blood gas sampling and the associated length
of mechanical ventilation in children with respiratory failure from
bronchiolitis who are initiated on mechanical ventilation.
Material and Methods
In this study, we conducted a retrospective review of patients
with an admission diagnosis of respiratory failure secondary
to bronchiolitis admitted to Cohen Children’s Medical Center
of NY (CCMC) PICU. Inclusion criteria included age 0 to 2 years,
diagnosis of bronchiolitis requiring mechanical ventilation, and
admission between May, 2008 and June, 2014. Patients with a
primary or secondary diagnosis of pneumonia, required inotropes
or vasopressors and/or extracorporeal membrane oxygenation
were excluded. Data collected included age, gender, history of
prematurity, duration of mechanical ventilation, presence of chronic comorbidities, presence of an arterial cannulas, number
and type of blood gases drawn, and any arterial cannula related
complications (e.g. thrombosis). Patients were divided into
one of two cohorts depending on whether or not they had an
arterial cannula placed after admission for respiratory failure and
initiation of mechanical ventilation.
To compare disease severity of the two groups, heart rate
(HR), respiratory rate (RR), and SpO2/FiO2 ratio calculated at
the time of intubation were recorded. In the A-line group, HR, RR
and PaO2/FiO2 ratios were also calculated at the time of arterial
catheter placement. For the cohort of patients without arterial
catheter or arterial blood gas sampling, the PaO2 was estimated
from the oxygen hemoglobin dissociation curve using the last
recorded oxygen saturation prior to intubation as outlined by
Aboab et al. [9] and Brockway et al. [10] Categorical variables
were analyzed using the Fisher exact test and continuous
variables were analyzed using a t-test (Minitab 14). A p< 0.05 was
considered statistically significant. The study was approved by the
North Shore Long Island Jewish Institutional Review Board (IRB).
Results
109 patients met inclusion criteria and 76 (70%) had an
arterial catheter. In the arterial catheter cohort, mean age was
7.6 months, 58% were male, 43% had a history of prematurity,
and 46% had comorbidities. Table 1 shows that for the group of
patients without an arterial cannula, the mean age was 6 months
(p = 0.24), 61% were male (p= 0.84), 42 % had a history of were
prematurity (p = 1.0), and 64% had comorbidities (p = 0.1). The
chronic comorbidities in both cohorts included chronic lung
disease, cerebral palsy, congenital heart disease (Ventricular
Septal defect and coarctation), Down’s syndrome and DiGeorge
syndrome. No arterial catheter related complications were
reported.
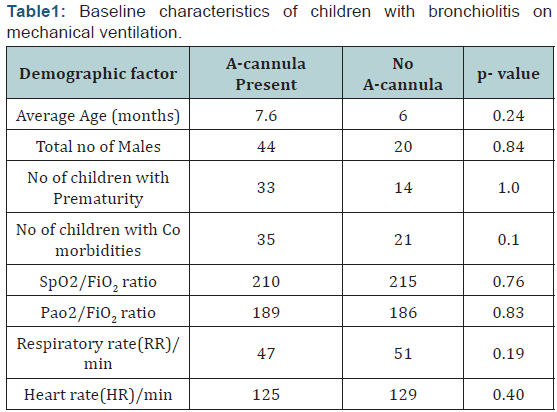
The last documented HR, RR, PaO2/FiO2 and SpO2/FiO2
ratios prior to intubation were recorded for each patient included
in the study analysis. The two cohorts were compared by a student
t-test to determine whether the severity of illness between the two cohorts were similar as shown in (Table 1). In the cohort of
patients with an arterial cannula, the cannula was placed within 2
hours of the patient intubation. The p-value for each demographic
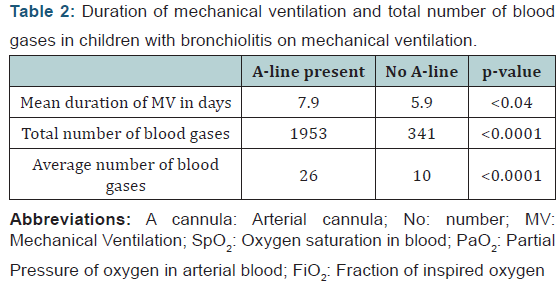
and disease characteristic was not significant. Table 2 shows that
the difference in mean duration of mechanical ventilation and the
total and average number of blood gases drawn in both the groups
were statistically significant.
Discussion
To date, this is the first study to examine the duration of
mechanical ventilation in children intubated for bronchiolitis
managed with and without an arterial cannula for frequent
blood gas sampling. Our analysis suggests children intubated for
respiratory failure secondary to bronchiolitis may be managed
successfully without the insertion of an arterial cannula and
frequent sampling of ABGs. The mean duration of mechanical
ventilation in the arterial cannula group in our study was
equivalent to previously reported length of intubation for a
child with bronchiolitis (8 ± 3 days), [11] indicating that our
arterial cannula group was typical in disease severity for patients
admitted for respiratory failure secondary to bronchiolitis. While
the duration of invasive mechanical ventilation was significantly
less in the cohort of children who did not have an arterial cannula,
they had similar HR, RR, PaO2/FiO2 and SaO2/FiO2 ratios at the
time of intubation.
Multiple studies have demonstrated that venous or capillary
blood gases are sufficient for approximating arterial pH, PCO2 and
HCO3 for patients requiring mechanical ventilation secondary
to respiratory failure in an intensive care unit, negating the need
for invasive arterial catheterization in these patients [12-16].
Additionally, non-invasive monitoring methods such as pulseoximetry
and end-tidal capnography utilized in conjunction with
infrequent capillary or venous sampling can be an alternative
strategy to frequent ABG sampling. Due to advent of these
technologies, indwelling arterial cannulas are less commonly
utilized [17].
Despite the costs and potential risks of arterial cannulas
and the presence of non-invasive monitoring methods, the use
of arterial cannulas for monitoring of patients with respiratory
failure remains common [18]. Furthermore, it remains unclear
if the presence of arterial cannulas and frequent ABG sampling
improves patient outcome [19]. In a review of a multicenter clinical trial on the use of prone positioning for pediatric acute
lung injury, Khemani et al. [20] demonstrated that of over 11,000
intubated and mechanically ventilated children, at least 15%
did not have an arterial cannula. Interestingly, those without an
arterial cannula received a similar level of mechanical ventilator
support compared to children with an arterial cannula suggesting
that the presence of arterial blood sampling was not associated
with substantial difference in mechanical ventilation management
strategies [20].
In our single center retrospective cohort study we found that
the presence of an arterial cannula was associated with a longer
duration of mechanical ventilation than the cohort managed
without an arterial cannula. There are many possible reasons that
may account for this finding. One possibility may be that weaning
mechanical ventilation utilizing blood gas sampling adds delay
due to the time required for the laboratory results to be completed
and reported. Another possibility might be that details from the
arterial blood gas such as an exact PaO2 or pH and PaCO2 may delay
the pace of weaning if blood gas results rather than assessment of
the work of breathing is given precedence. These results suggest
that the presence of arterial cannulas and frequent ABG sampling
may not have benefit in the care of patients with bronchiolitis and
respiratory failure and is, in our study, associated with a longer
duration of mechanical ventilation compared to a cohort with
similar indices of respiratory illness but without arterial cannulas.
Lewis et al. [6] demonstrated that the presence of an arterial
cannula is associated with increased blood draws in patients in the
ICU. In our study, we found that the average number of blood gases
drawn was 2.5 times higher in the cohort with an arterial cannula
compared with the cohort without an arterial cannula (p<0.0001).
Our findings suggest that in addition to a lack of an association of
benefit in children with arterial cannulas with respect to duration
of mechanical ventilation, the catheters contribute to a greater
number of blood draws for blood gas sampling.
While our results were significant and warrant further
prospective studies evaluating the benefits of ABG sampling in
children mechanically ventilated for bronchiolitis, we recognize
our analysis has limitations. Our study was a retrospective
cohort design of a single center and there may be factors such as
individual clinician variability in mechanical ventilation weaning
practice. However, our multi-disciplinary ICU, much like others,
takes a team based approach to the management of our patients
and multiple attendings, critical care fellows, residents and nurses
play a collaborative role in the care of each patient. Additionally, it
is possible that our two study cohorts of bronchiolitic respiratory
failure had different epidemiologies of viral triggers. While this is
certainly possible given that only a small number of bronchiolitis
associated viruses are routinely screened for, we do not believe
that such a bias is likely given that there has never been a policy or
practice in our ICU requiring arterial cannula placement based on
associated virus or any other epidemiologic facet of bronchiolitis.
While we believe that our choice of how to compare severity of lung disease in the two groups is consistent with accepted
practice in the literature, we did extrapolate PaO2 from an SpO2
for the group managed without arterial cannulas. This practice of
extrapolation has precedence in that a recent large multicenter
clinical trial of sedation management for respiratory failure in
children utilized the same methodology in reporting their results
[21]. Additionally, the recent publication of consensus definitional
criteria for pediatric acute respiratory distress syndrome has
advocated the use of SpO2/FiO2 rather than PaO2 in the absence
of invasive monitoring [22]. Additionally, while the timing of the
vital sign measurements in our analysis were within 2 hours of
intubation for all patients, it is possible some patients’ clinical
status changed appreciably in that interval and there level of
illness was not accurately represented by our data.
Conclusion
In our retrospective cohort study in children managed with
and without arterial cannulas and ABG sampling, the presence
of arterial cannulas was associated with a longer duration of
mechanical ventilation and increased frequency of blood gas
sampling. There are substantial risks that are associated with
the arterial cannulas that may outweigh the putative benefits.
Significant consideration should be given to the need for
placement of arterial cannulas in the management of children
with bronchiolitis requiring invasive mechanical ventilation.
Further studies evaluating the risk versus benefit of invasive
monitoring, such as arterial line cannulas, in common critical
illness is warranted.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment