Analysis of Tools for Diagnosing Autism Spectrum Disorder in the Indian Context-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Autism Spectrum Disorder (ASD) is a
neurodevelopmental condition with varied manifestations and poses a
diagnostic challenge. The prevalence of ASD has increased in a highly
populated and demographically ‘young’ country like India. However,
prevalence rates are varied due to differences in measurement methods.
Moreover, caregivers tend to delay reporting for developmental concerns
as compared to physical health problems. The current analysis focuses on
two common diagnostic tools used in India for ASD i.e. the fifth
edition of the Diagnostic and Statistical Manual of Mental Disorders and
the Indian Scale for Assessment of Autism; and compares these tools
with the revised Autism Diagnostic Interview. The analysis describes
strengths and limitations of each of these tools and provides
recommendations for their use in outpatient clinical practice.
Keywords: Autism Spectrum Disorder; Diagnosis; Analysis; India, DSM-5; ADI-R; ISAAAbbreviations: ASD: Autism Spectrum Disorder; ISAA: Indian Scale for Assessment of Autism; ADI: Autism Diagnostic Interview
Introduction
Autism Spectrum Disorder (ASD) is a
neurodevelopmental condition with highly varied manifestations and poses
a diagnostic challenge. First, as per the fifth edition of the
Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the
current definition of ASD broadly includes features of previously known
conditions such as ‘classic autism’ (or Kanner’s autism), childhood
disintegrative disorder, pervasive developmental disorder-not otherwise
specified, as well as Asperger syndrome [1]. Although individuals with
ASD have persistent deficits in social communication and interaction, as
well as restricted and/or repetitive behaviors, the clinical features
are part of a ‘spectrum’ i.e. each individual has different degrees of
impairment, marked by combination of symptoms of varying severity [2].
Second, the etiological approach to diagnosing ASD (unlike several other
physical or mental health conditions) is impractical. Genetic risk
factors have been implicated to cause ASD [3], as also intake of
valproic acid and thalidomide in pregnancy [4-5], in addition to routine
perinatal complications [6], increased parental age [7] and birth
defects associated with dysfunction of the central nervous system [8].
Definitive evidence on implicating these risk factors as causative
agents has not been established. Third, in the Indian context,
caregivers tend to delay reporting of developmental concerns, as
compared to physical health problems [9]. Thus, initial evaluation or
diagnostic impression of ASD needs to be comprehensive and
individualized to the child’s needs – and not merely sensitive in
detecting the condition. This is decisive in framing the goals and
strategies of an intervention program.
Finally, from an epidemiological perspective, the
prevalence of ASD has increased in a highly populated and
demographically ‘young’ country like India. However, prevalence rates
are varied due to differences in measurement tools [10-12]. Studies have
reported prevalence of 1 in 65 children (2-9 years of age, 4000
households), 1 in 500 children (1-9 years of age, 5000 households) and 1
in 1000 children (1-10 years of age, 11,000 children) in different
regions of India. These differences have failed to define the burden of
ASD in the Indian context. Thus, we need a discussion on strengths and
challenges of diagnostic tools for high-prevalence developmental
disorders like ASD, to have a standardized evaluation approach.
The current analysis focuses on two common diagnostic
tools used in India for ASD i.e. the DSM-5 and the Indian Scale for
Assessment of Autism (ISAA); and compares these methods with the revised
Autism Diagnostic Interview (ADI-R).
A diagnostic tool needs to be culturally relevant, with optimum
sensitivity and specificity. The assessment should exert minimum
demand on professionals, in terms of their required training to use
the tool. It should be feasible to administer in a clinic setting, based
on time and costs. Finally, it should be comprehensive i.e. covering
maximum aspects of the developmental-behavioral profile of
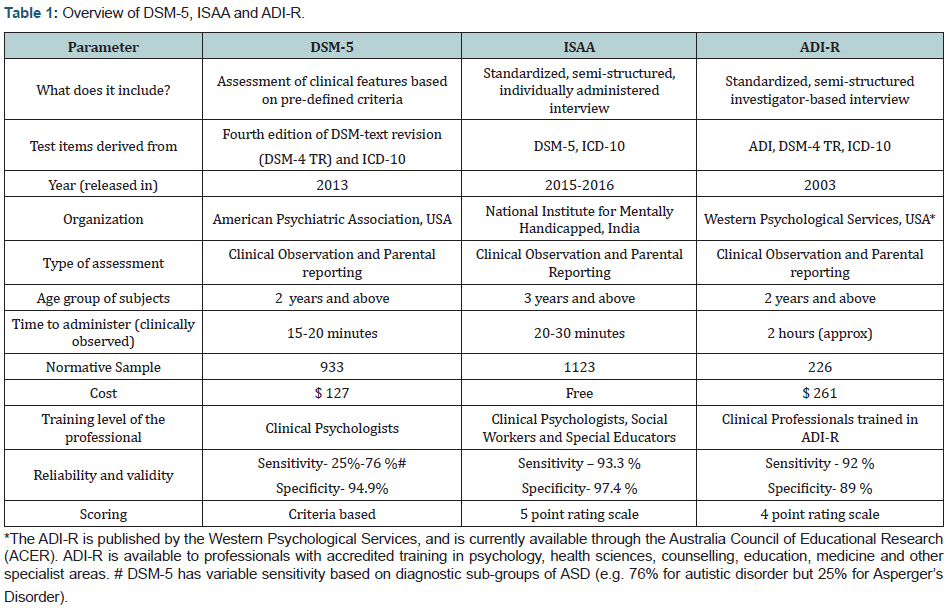
ASD. (Table 1) provides an overview of DSM-5 [1,2,13,14], ISAA
[2,15,16] and ADI-R [17-19].
Analysis of strengths and weaknesses of diagnostic tools:
DSM-5: The strengths of DSM-5 include: (1) DSM-5
provides ‘specifiers’ in addition to the diagnostic impression and
level of severity. The specifiers include accompanying language
impairment; intellectual impairment; associated medical or
genetic conditions or environmental factors; associated neuro developmental, mental or behavioral disorders and catatonia.
Thus, DSM-5 creates scope to identify associated conditions along
with the primary diagnosis.(2) DSM-5 provides severity level for
each criterion (e.g. severity of deficits in social interaction and
communication). (3) DSM-5 can be most rapidly administered, out
of the three diagnostic tools.
Following are the limitations of DSM-5: 1) All previously
defined disorders related to Autism have been grouped under
‘ASD’, which not only reduces the sensitivity (Table 1) particularly
in younger children, but also limits the clinician to fully understand
the (former) clinical sub-types (e.g. pervasive developmental
disorder-not otherwise specified, Asperger’s Disorder, Rett
syndrome, childhood disintegrative disorder, etc.). This limits the
individualization of an intervention plan to the child’s needs. 2)
DSM-5 does not specify the age-range for emergence of symptoms.
It states that ‘symptoms may not be fully manifest until social
demands exceed capacity’ [20].
ISAA: The strengths of ISAA include:
1) ISAA scores
symptoms through a five-point rating scale, which categorizes the
symptom-frequency (i.e. rarely, sometimes, frequently, mostly and
always). Percentages have been pre-assigned to these categories
based on the validation processes implemented to prepare the
scale [16]. Thus, the categorization improves the specificity of
caregiver’s reporting. 2) An important advantage of ISAA (and
the rationale for its design) is its standardization and cultural
relevance to the Indian population. 3) ISAA can be administered by
professionals besides psychologists, which potentially widens its
applicability in a high-prevalence region like India. 4) Along with
observation and parental interview, ISAA also includes ‘testing’
i.e. the scale has recommended certain activities requiring clinicbased
materials, which can be performed to elicit a response from
the child suspected to have ASD [16]. Several of these materials
are home-based. 5) ISAA provides disability certification based on
scoring. It has been anecdotally observed that such a certification
process, in-built within assessment techniques, has encouraged parents
to report for early intervention in other developed
countries. However, evidence for the same is lacking in the Indian
context. 6) ISAA has the highest specificity out of the three scales.
7) ISAA is free of cost and available in regional Indian languages.
The limitations are as follows: 1) Articulation of some
items, in the ‘Observation and Interview’ section of ISAA is not
adequately clear. This may necessitate the administrator to refer
the manual during evaluation. Examples of few such items include:
“(individual) has unusual vision”, “has unusual memory of some
kind”, “engages in self-stimulating emotions”, “shows exaggerated
emotions” and “shows inappropriate emotional responses”. 2)
ISAA provides a summative diagnosis i.e. an overall score that
categorizes the condition as ‘no’, ‘mild’, ‘moderate’ or ‘severe’
Autism. Thus, no specific severity levels have been provided for
individual sub-domains (i.e. social relationship and reciprocity,
emotional responsiveness, speech language and communication,
behavior patterns, sensory aspects and cognitive component).
3) ISAA can identify Autism only in 3-9 year old children and
certify disability of at least 40%. Further research is warranted to
evaluate its diagnostic value in 2-3 year old children [21].
ADI-R: The strengths of ADI-R include: 1) ADI-R has the
widest age-range out of the three scales. Two diagnostic algorithms
are available for children 2 to less than 4 years of age, and 4 years
and older. Moreover, new algorithms have been made for children
12-47 months of age and those with non-verbal mental age of 10
months, to increase its application [22]. 2) ADI-R provides a score-based
severity level for each domain (unlike DSM-5 that provides
a clinical judgment-based severity level). 3) ADI-R includes the
most number of testing items - 93 items distributed across five
sections i.e. introduction, communication, social development
and play, repetitive and restricted behaviors and general behavior
problems. Thus, due to its detailed nature (viz. items and severity
levels), ADI-R provides the greatest breadth of information
to locate the affected developmental domains in a child, for
designing the most suitable intervention program. 4) ADI-R is
a parent-friendly interview, since the questions are ordered
in such a way that caregivers can inform positive aspects of the
child’s behavior, which reduces the discomfort of giving repeated
answers on negative behaviors. 5) Most items are rated separately
for ‘current’ behavior of the child; as well as the period in child’s
early life, during which the behavior in question was most atypical.
Hence, the degree of detail is not only in the description of current
symptoms, but also their emergence in early life, thus increasing
credibility of the diagnostic impression. 6) ADI-R includes ‘notapplicable’
and ‘not-known’ codes for items (in contrast to >DSM-5
and ISAA) which reduce the bias in scoring items that could be
developmentally irrelevant.
In terms of limitations, ADI-R is the most expensive and
time-consuming of the three tools, apart from the lack of cultural
validation in the Indian context, and the fact that it needs
specialized training, which may take at least two months to
complete [23]. Moreover, in the Indian context, caregivers tend
to focus more on physical health of the child, rather than mental health. Greater emphasis is placed on aspects like academic
ability; while behaviors related to play and social interaction are
often overlooked. Hence, responses by caregivers to the detailed number of items, may not always be appropriate[24].
Conclusion
The analysis compares three common tools for diagnosing
ASD, in a context where screening alone may have little value,
due to delayed identification of ASD and delayed reporting by
caregivers. The authors propose that studies should be conducted
to establish the specific indications where a DSM-5 or an ISAA
will be more appropriate for diagnosis. Studies should also be
conducted to validate ISAA in children younger than two years. In
addition, there is a strong need to revise the articulation of some
items in ISAA that may not be well understood. Moreover, since
ISAA also involves testing, additional training maybe required
for evaluation of certain domains, such as sensory aspects and
cognitive component. In these cases, it will be more appropriate
to modify some components of ISAA, so that professionals of
different skill-sets can use the scale, for example – pediatricians,
physicians, psychologists, special educators and medical social
workers. In contrast, ADI-R mandates formal training and DSM-5
mandates administration only by psychologists.
ADI-R may not be suitable for routine use, given the timeconstraints
in developmental pediatric practice and the cultural
incompatibility with the Indian context. With regard to the latter,
however, it may be an assessment of choice for urban middle-income
and upper-income families. Moreover, there are frequent
situations where a child may have features of ASD but diagnostic
criteria are not met in DSM-5. Such situations could arise in the
use of ISAA as well. Hence, practitioners should take advantage
of the detailed number of items and scoring strata in ADI-R, for
evaluating such children. To that end, the therapy centre needs
to have a trained professional who can administer ADI-R and has
pre-tested the method with Indian parents in order to locate any
items which need modification, based on cultural factors.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment